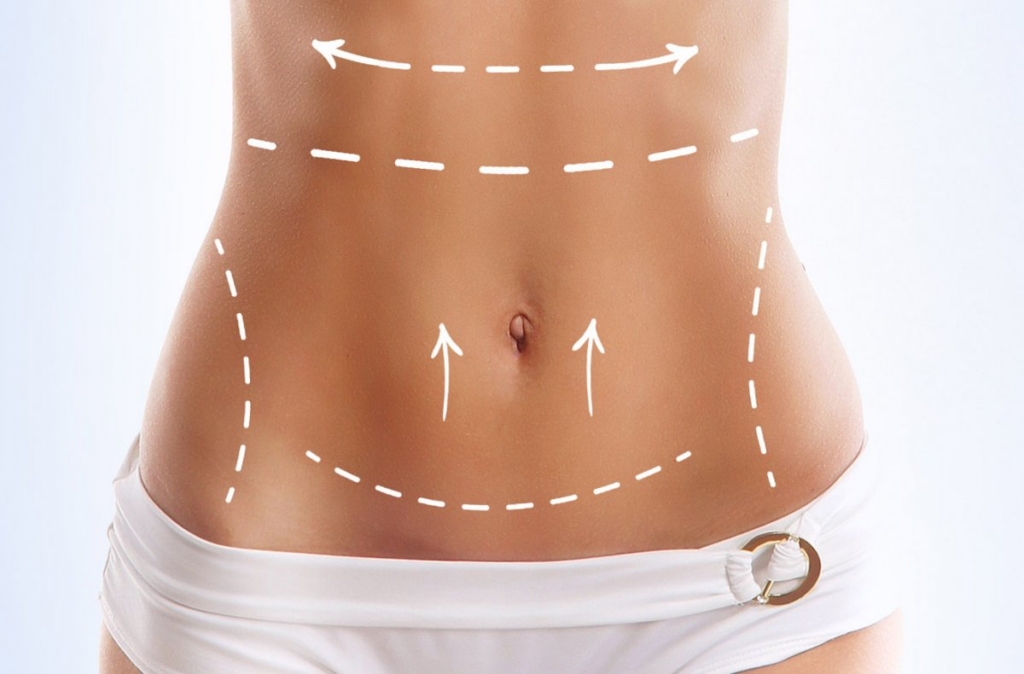
Undergoing abdominoplasty, commonly known as a tummy tuck, is a significant decision for many individuals seeking a more contoured and aesthetically pleasing abdominal profile. This transformative surgical procedure effectively removes excess skin and fat, and often tightens weakened abdominal muscles, leading to remarkable improvements in body shape. However, the journey to a flatter, firmer abdomen does not always conclude immediately after the surgery. A common, yet often concerning, aspect of the post-operative period is the development of lumps or areas of hardness in the treated region. These lumps can range from minor, temporary swelling to more persistent formations, and understanding their nature is paramount for a smooth and reassuring recovery.
The appearance of unexpected textures beneath the skin can naturally cause anxiety for patients who have invested significantly in their physical transformation. It is crucial to recognize that while some degree of firmness or irregularity is a normal part of the healing process, certain types of lumps may require medical attention. This comprehensive guide aims to demystify the various causes behind these post-abdominoplasty lumps, offering a deep dive into their mechanistic details, real-world implications, and the most effective strategies for both their management and prevention. By providing clear, actionable insights, we empower patients to navigate their recovery with confidence, fostering informed discussions with their surgical teams and ensuring the best possible long-term outcomes.
Our central thesis is that a thorough understanding of post-abdominoplasty lumps is not merely about identifying a problem, but about embracing a proactive approach to healing. This involves recognizing the subtle signs, understanding the underlying physiological processes, and knowing when and how to seek professional guidance. From the initial stages of fluid accumulation to the more complex development of scar tissue or fat necrosis, each type of lump presents unique characteristics and requires tailored care. This article will serve as an authoritative resource, meticulously detailing the core principles of lump formation, exploring various treatment modalities, and emphasizing the critical role of diligent postoperative care. Ultimately, our goal is to equip you with the knowledge necessary to achieve not just an aesthetically pleasing result, but also a healthy, comfortable, and fully recovered abdomen.
The journey through abdominoplasty recovery is a testament to patience and adherence to medical advice. While the initial excitement of a new silhouette is palpable, the reality of healing involves a series of biological responses that can manifest in unexpected ways. Lumps, whether soft and fluid-filled or firm and fibrous, are often indicators of these intricate healing processes. By shedding light on these phenomena, we aim to alleviate common fears and provide a roadmap for effective intervention. This includes distinguishing between benign, self-resolving conditions and those that necessitate clinical assessment. We will also explore the psychological impact of these concerns, advocating for open communication and robust support systems to ensure holistic well-being throughout the recovery period. The insights presented here are designed to transform uncertainty into understanding, paving the way for a truly optimal post-surgical experience.
Furthermore, this guide extends beyond immediate post-operative concerns to consider the long-term implications and future outlook for patients. Maintaining the results of an abdominoplasty and managing any persistent issues requires ongoing commitment to a healthy lifestyle and regular follow-up with your plastic surgeon. We will discuss how factors such as weight stability and continued adherence to a balanced diet and exercise regimen contribute to the durability of your surgical outcome. By integrating comprehensive information on prevention, treatment, and sustained care, this article offers a definitive resource for anyone navigating the complexities of post-abdominoplasty recovery. Our commitment is to provide clarity and expert guidance, ensuring that your journey towards a revitalized self is as smooth and successful as possible.

Sommario
Understanding the Nature of Post-Abdominoplasty Lumps
The appearance of lumps after abdominoplasty is a common concern, yet many of these formations are a normal part of the body’s healing process. Distinguishing between different types of lumps is crucial for appropriate management and peace of mind. These post-surgical irregularities can manifest in various forms, each with distinct characteristics and underlying causes (Ruli, 2025a).
Seromas: Fluid Accumulation
One of the most frequent causes of post-operative lumps is a seroma, which is an excessive accumulation of fluid under the skin (Mayo Clinic Staff, 2025). This fluid, primarily lymphatic fluid and sometimes blood plasma, collects in the space created during surgery where tissue has been removed. Seromas typically feel soft, spongy, or fluctuant to the touch and can range in size from small, localized pockets to larger, more noticeable swellings. They often develop a few days to several weeks after surgery. The American Society of Plastic Surgeons (n.d.) notes that drainage tubes are often used after surgery to help minimize the risk of seroma formation, and sometimes surgical techniques are employed to reduce this risk.
Hematomas: Blood Collection
Similar to seromas, hematomas involve fluid collection, but specifically refer to a localized collection of blood outside of blood vessels (Tri Valley Plastic Surgery, n.d.). These can occur if small blood vessels continue to bleed after surgery. Hematomas typically present as firm, tender, and often discolored lumps (blue or purple) and usually appear earlier in the post-operative period than seromas. While smaller hematomas may resolve on their own, larger ones often require drainage to prevent complications and promote proper healing (Ruli, 2025a).
Scar Tissue (Fibrosis)
As the body heals, it naturally produces scar tissue to repair incisions. This process, known as fibrosis, can sometimes lead to the formation of hard, firm lumps beneath the skin (Ruli, 2025a). These lumps are essentially dense collagen fibers that form as part of the wound healing response. While all surgical incisions result in some degree of scar tissue, excessive or improperly formed scar tissue can feel like a lump. In some cases, this can evolve into hypertrophic scars or keloids, which are raised and thickened scars, though these are more about the visible scar itself rather than deep internal lumps. Scar tissue lumps tend to be firm and can be sensitive to touch, often developing weeks to months after surgery as the deeper tissues mature.
Fat Necrosis: Damaged Fatty Tissue
Fat necrosis occurs when fatty tissue in the treated area loses its blood supply and dies (Tri Valley Plastic Surgery, n.d.). This can result in the formation of hard, irregular lumps that may feel firm or rubbery. While rare, it is a potential complication, especially in areas where significant fat removal or manipulation has occurred. The Mayo Clinic Staff (2025) notes that tissue damage, including fatty tissue, is a risk, and smoking can increase this risk. Depending on the size, fat necrosis may resolve on its own, or in some cases, may require intervention.
Suture Granulomas: Reaction to Sutures
Occasionally, the body may react to the dissolvable sutures used internally during abdominoplasty, leading to the formation of small, hard lumps known as suture granulomas (Ruli, 2025a). These are essentially inflammatory responses to the foreign material (the suture). They are typically small, firm, and localized, often appearing along the incision lines or where internal sutures were placed. While generally benign, they can sometimes cause discomfort or be noticeable through the skin.
Swelling and Inflammation
General swelling and inflammation are normal and expected components of the post-surgical healing process. While not a distinct “lump” in the same way as a seroma or fat necrosis, significant swelling can make the abdominal area feel hard, firm, and uneven (Ruli, 2025a). This generalized hardness is often most pronounced in the initial weeks following surgery and gradually subsides as the body heals and fluid retention decreases. Compression garments play a vital role in managing this swelling and promoting a smoother contour (Ruli, 2025c).

The Science Behind Lump Formation: A Deeper Dive
To truly understand post-abdominoplasty lumps, it is beneficial to delve into the intricate biological processes that underpin their formation. The body’s response to surgical trauma is a complex cascade of events designed to repair damaged tissues, and sometimes, these reparative mechanisms can lead to palpable irregularities.
Physiological Response to Trauma
Any surgical procedure, including abdominoplasty, initiates a wound healing response. This involves several overlapping phases: inflammation, proliferation, and remodeling. In the inflammatory phase, blood vessels dilate, and immune cells rush to the site to clear debris and fight potential infection. This initial response contributes to swelling and tenderness. The proliferative phase involves the formation of new tissue, including collagen, to close the wound. Finally, the remodeling phase, which can last for months or even years, involves the reorganization and strengthening of the newly formed collagen (Ruli, 2025c).
Role of the Lymphatic System
The lymphatic system is a critical network of vessels and nodes responsible for draining excess fluid, waste products, and immune cells from tissues. During abdominoplasty, lymphatic vessels in the abdominal area are inevitably disrupted. This disruption can impair the normal drainage of interstitial fluid, leading to its accumulation in the surgical space, which manifests as a seroma (Mayo Clinic Staff, 2025). The body attempts to re-establish lymphatic pathways, but this takes time, making seroma formation a relatively common early post-operative complication.
Collagen Production and Remodeling
Scar tissue, or fibrosis, is primarily composed of collagen, a structural protein. During the proliferative phase of healing, fibroblasts produce large amounts of collagen to bridge the surgical gap. In the remodeling phase, this collagen is reorganized and strengthened. However, sometimes this process can be overactive or disorganized, leading to an excess accumulation of collagen that forms a palpable lump. This is particularly true for hypertrophic scars and keloids, where collagen production outpaces degradation, resulting in raised, firm areas (Ruli, 2025a). The firmness of these lumps is directly related to the density and arrangement of these collagen fibers.
Vascular Compromise and Fat Viability
Fat necrosis occurs when the blood supply to a section of fatty tissue is compromised. During abdominoplasty, especially with extensive undermining or liposuction, the delicate blood vessels supplying the fat can be damaged. If a portion of fat does not receive adequate oxygen and nutrients, its cells die. The body then attempts to clear this dead tissue, which can lead to an inflammatory response and the formation of a firm, often calcified, lump (Tri Valley Plastic Surgery, n.d.). Factors like smoking significantly increase the risk of vascular compromise and, consequently, fat necrosis (Mayo Clinic Staff, 2025).

Early Detection and Diagnosis: When to Seek Professional Guidance
While some post-operative lumps are benign and resolve with time, others may indicate a complication requiring medical intervention. Early detection and accurate diagnosis are crucial for effective management and to ensure the best possible recovery outcome. Patients play a vital role in this process by being vigilant and communicating any concerns to their surgical team.
Recognizing Concerning Signs
It is important to monitor your body for specific signs that may indicate a more serious issue. While mild discomfort and swelling are normal, you should seek professional advice if you experience:
- Persistent or increasing pain: Pain that worsens over time or is not relieved by prescribed medication.
- Rapidly increasing size or hardness of a lump: A lump that grows quickly or becomes significantly firmer.
- Redness or warmth: Localized redness or warmth around a lump, which could indicate infection or inflammation.
- Fever or chills: Systemic signs of infection.
- Pus or foul-smelling discharge: Any drainage from the incision site that is not clear or light pink.
- Delayed wound healing: Incisions that do not seem to be closing or appear to be opening up (Ruli, 2025a; Mayo Clinic Staff, 2025).
Importance of Regular Follow-up Appointments
Scheduled follow-up appointments with your plastic surgeon are not merely routine; they are critical for monitoring your healing progress and identifying any potential complications early. During these visits, your surgeon will perform a physical examination, assess the surgical sites, and address any concerns you may have. These appointments provide an opportunity for your surgeon to detect subtle changes that you might not notice yourself and to initiate appropriate interventions promptly (Ruli, 2025c).
Diagnostic Tools
In addition to a thorough physical examination, your surgeon may utilize diagnostic tools to accurately assess the nature of a lump:
- Esame fisico: The surgeon will palpate the area to determine the size, consistency, tenderness, and mobility of the lump. This initial assessment often provides significant clues about its underlying cause.
- Ultrasound: An ultrasound scan is a non-invasive imaging technique that can differentiate between fluid collections (seromas, hematomas) and solid masses (scar tissue, fat necrosis). It provides real-time images and can guide aspiration procedures if necessary.
- Aspiration: For fluid-filled lumps, a fine needle aspiration can be performed to both diagnose and treat the condition. The aspirated fluid can also be sent for laboratory analysis to rule out infection (Ruli, 2025a).

Comprehensive Management Strategies for Post-Surgical Lumps
Once a lump has been identified and diagnosed, a tailored management plan can be implemented. Treatment approaches vary significantly depending on the type, size, and symptoms associated with the lump. Both conservative and medical interventions play a role in achieving optimal resolution.
Conservative Approaches
Many post-operative lumps can be effectively managed with non-invasive techniques, particularly in the early stages of recovery.
- Indumenti a compressione: Wearing a compression garment as advised by your surgeon is a cornerstone of post-abdominoplasty care. These garments apply gentle, consistent pressure to the surgical area, which helps to reduce swelling, minimize fluid accumulation (seroma formation), and support the healing tissues. The continuous compression also aids in contouring the abdomen and can help flatten developing scar tissue (Ruli, 2025a; Mayo Clinic Staff, 2025).
- Manual Lymphatic Drainage (MLD) Massage: This specialized, gentle massage technique is designed to stimulate the lymphatic system, encouraging the drainage of excess fluid and reducing swelling. MLD can be particularly beneficial for seromas and generalized post-operative edema. It helps to improve circulation and can soften scar tissue over time. It is crucial that MLD is performed by a certified therapist experienced in post-surgical care to ensure proper technique and avoid exacerbating the condition (Ruli, 2025a).
- Topical Treatments: For scar tissue lumps, various topical treatments can be beneficial. Silicone-based gels or sheets are widely recommended for improving scar appearance and reducing hardness. They work by hydrating the scar tissue and regulating collagen production. Creams or ointments containing ingredients like vitamin E or cocoa butter are also sometimes suggested for their moisturizing and skin-softening properties, though scientific evidence for their efficacy in reducing scar tissue lumps is less robust than for silicone products (Ruli, 2025a).
Medical Interventions
When conservative methods are insufficient or for certain types of lumps, medical interventions may be necessary.
- Aspiration/Drainage: For seromas and hematomas, the most direct treatment is aspiration, where a surgeon uses a needle and syringe to drain the accumulated fluid (Ruli, 2025a; Mayo Clinic Staff, 2025). This procedure is typically quick and can provide immediate relief from pressure and discomfort. Multiple aspirations may be required for recurrent seromas.
- Corticosteroid Injections: For persistent or problematic scar tissue lumps, corticosteroid injections can be administered directly into the lump. Corticosteroids are powerful anti-inflammatory agents that help to reduce inflammation and break down excess collagen, thereby softening and flattening the scar tissue (Ruli, 2025a).
- Sclerotherapy: In some cases of recurrent seromas, particularly those that are large and persistent, sclerotherapy may be considered. This involves injecting a sclerosing agent into the seroma cavity, which causes the walls of the cavity to stick together, preventing further fluid accumulation (Ruli, 2025a).
- Antibiotics: If a lump is accompanied by signs of infection (redness, warmth, pus, fever), antibiotics will be prescribed to treat the bacterial infection (Mayo Clinic Staff, 2025).
Surgical Revision
In rare instances, if lumps persist despite conservative and medical treatments, or if they significantly impact the aesthetic outcome or cause ongoing discomfort, surgical revision may be an option. This could involve excising problematic scar tissue, removing areas of fat necrosis, or addressing any underlying structural issues contributing to the lump formation (Ruli, 2025a). The decision for surgical revision is made in close consultation with your plastic surgeon, weighing the benefits against the risks of further surgery.
Proactive Prevention: Minimizing the Risk of Lumps
While some degree of lumpiness can be an unavoidable part of the healing process, several proactive measures can significantly minimize the risk of developing problematic lumps after abdominoplasty. These strategies encompass careful surgical planning, diligent post-operative adherence, and a commitment to overall health.
Choosing an Experienced and Board-Certified Surgeon
The foundation of a successful abdominoplasty with minimal complications lies in selecting a highly qualified and experienced plastic surgeon. A board-certified plastic surgeon possesses the extensive training, anatomical knowledge, and surgical skill necessary to perform the procedure with precision, minimizing trauma to tissues and optimizing healing. Their expertise in proper surgical techniques, including careful tissue handling and meticulous closure, directly contributes to reducing the likelihood of complications like seromas, hematomas, and excessive scar tissue formation (Ruli, 2025c).
Adhering to Postoperative Instructions Diligently
Strict adherence to your surgeon’s post-operative instructions is paramount for a smooth recovery and to prevent complications. These instructions are specifically designed to support optimal healing and include guidance on:
- Wearing Compression Garments: As discussed, compression garments are vital for reducing swelling and preventing fluid accumulation. Consistent wear, as directed, is crucial (Ruli, 2025a; Mayo Clinic Staff, 2025).
- Limitazioni delle attività: Avoiding strenuous activities, heavy lifting, and movements that strain the abdominal muscles during the initial recovery period is essential. Premature or excessive activity can disrupt healing, increase swelling, and potentially lead to seroma or hematoma formation (Ruli, 2025a; Mayo Clinic Staff, 2025).
- Cura delle ferite: Following precise instructions for cleaning incisions and changing dressings helps prevent infection, which can contribute to inflammation and lump formation (Ruli, 2025c).
Maintaining a Healthy Lifestyle
Your overall health significantly impacts your body’s ability to heal and recover. A healthy lifestyle before and after surgery can minimize risks:
- Nutrition and Hydration: A balanced diet rich in protein, vitamins, and minerals supports tissue repair and immune function. Adequate hydration is also crucial for overall healing (Ruli, 2025c).
- Smoking Cessation: Smoking severely impairs blood flow and oxygen delivery to tissues, significantly increasing the risk of poor wound healing, infection, and fat necrosis. Quitting smoking well in advance of surgery and throughout the recovery period is critical for optimal results (Ruli, 2025c; Mayo Clinic Staff, 2025).
- Stable Weight: Significant weight fluctuations after abdominoplasty can compromise the long-term results and potentially lead to new areas of laxity or unevenness. Maintaining a stable weight is key to preserving your contoured abdomen (American Society of Plastic Surgeons, n.d.; Mayo Clinic Staff, 2025).
Thorough Preoperative Evaluation
A comprehensive preoperative evaluation allows your surgeon to assess your overall health, identify any underlying conditions, and discuss potential risk factors. This includes reviewing your medical history, current medications, and lifestyle habits. Addressing any pre-existing conditions or modifying certain behaviors (like smoking) before surgery can significantly reduce the risk of complications, including lump formation (Ruli, 2025c; Mayo Clinic Staff, 2025).
Psychological Impact and Support During Recovery
The physical recovery from abdominoplasty is often accompanied by a significant emotional and psychological journey. The appearance of unexpected lumps or irregularities can be a source of considerable anxiety, impacting a patient’s overall satisfaction and mental well-being. Addressing these emotional aspects is as crucial as managing the physical symptoms.
Addressing Patient Anxiety and Concerns
Patients often have high expectations for their abdominoplasty results, and any deviation from the anticipated smooth, flat contour can lead to distress. Lumps, even if benign, can trigger fears about the success of the surgery, potential complications, or long-term aesthetic outcomes. It is normal to feel worried, frustrated, or even regretful when facing these post-surgical concerns. Recognizing and validating these emotions is the first step towards effective coping.
Importance of Open Communication with the Surgical Team
Maintaining open and honest communication with your plastic surgeon and their team is paramount. Do not hesitate to voice any concerns, no matter how minor they may seem. Your surgical team is the most qualified resource to assess your condition, provide accurate information, and offer reassurance or appropriate interventions. Regular follow-up appointments are designed for these discussions, but you should feel comfortable reaching out between scheduled visits if new or worsening symptoms arise. Clear communication fosters trust and ensures that any issues are addressed promptly and effectively (Ruli, 2025a).
Support Groups and Mental Well-being
Connecting with others who have undergone similar procedures can provide invaluable emotional support. Online communities and local support groups offer platforms for sharing experiences, asking questions, and receiving encouragement from individuals who understand the unique challenges of post-surgical recovery. This peer support can help normalize feelings of anxiety and provide practical tips for coping. Additionally, if emotional distress becomes overwhelming, considering therapy or counseling can provide strategies for managing stress, anxiety, and body image concerns during this transformative period (Ruli, 2025a).
Long-Term Outlook and Future Considerations
The journey after abdominoplasty extends far beyond the initial recovery phase. The long-term outlook for managing post-surgical lumps is generally positive, with most resolving or significantly improving over time. However, maintaining the aesthetic and health benefits of the surgery requires ongoing commitment and awareness.
Typical Resolution Timeline
It is important to have realistic expectations regarding the timeline for the resolution of lumps. Many forms of post-operative swelling and minor irregularities will gradually subside within the first few weeks to months. Seromas, if aspirated, often resolve after one or more drainage procedures. Scar tissue maturation can take six to twelve months, or even longer, with the firmness and redness gradually diminishing over this period (Ruli, 2025a). Fat necrosis, if small, may also resolve spontaneously, though larger areas might persist or require intervention. Patience is a critical component of the recovery process, as the body needs ample time to heal and remodel tissues.
Maintaining Results: Stable Weight and Healthy Habits
The longevity of your abdominoplasty results, including the prevention of new irregularities, is closely linked to maintaining a stable weight and a healthy lifestyle. Significant weight fluctuations after surgery can stretch the skin and abdominal muscles again, potentially diminishing the positive outcome and even leading to new areas of laxity or unevenness (American Society of Plastic Surgeons, n.d.; Mayo Clinic Staff, 2025). A balanced diet and regular exercise regimen are not only beneficial for overall health but also crucial for preserving the contoured abdominal profile achieved through surgery. These habits support muscle tone and help prevent the accumulation of new fat deposits.
Potential for Recurrence and Ongoing Monitoring
While many lumps resolve, some conditions, particularly seromas, can recur. Ongoing monitoring of your abdominal area for any new or returning lumps is advisable. Regular self-examination and continued communication with your plastic surgeon during follow-up visits are essential for early detection and prompt management of any recurrent issues. Understanding that the body is a dynamic system, and healing is an ongoing process, helps in managing expectations and ensuring sustained positive results.
Conclusion: Empowering Your Abdominoplasty Recovery
The decision to undergo abdominoplasty is a deeply personal one, often driven by a desire for renewed confidence and a more harmonious body contour. While the prospect of a flatter, firmer abdomen is exciting, the reality of post-surgical recovery can sometimes present unexpected challenges, such as the formation of lumps. This comprehensive guide has illuminated the multifaceted nature of these post-abdominoplasty concerns, from the common fluid collections of seromas and hematomas to the more complex formations of scar tissue and fat necrosis. We have delved into the intricate biological mechanisms that underpin their development, emphasizing that these are often natural, albeit sometimes concerning, responses of the body to surgical trauma.
The journey to an optimal recovery is not a passive one; it demands proactive engagement and informed decision-making. We have underscored the critical importance of early detection, urging patients to be vigilant for any persistent or worsening symptoms and to communicate openly with their surgical teams. The array of management strategies, ranging from conservative approaches like compression garments and manual lymphatic drainage to medical interventions such as aspiration and corticosteroid injections, provides a clear pathway for addressing these lumps effectively. Furthermore, the emphasis on proactive prevention, including the judicious selection of a board-certified surgeon, diligent adherence to post-operative instructions, and a steadfast commitment to a healthy lifestyle, serves as a cornerstone for minimizing risks and fostering a smoother healing process.
Beyond the physical aspects, we have recognized the significant psychological impact that post-surgical irregularities can have on a patient’s emotional well-being. The anxieties and frustrations that may arise are valid, and fostering open communication with healthcare providers, alongside seeking support from peer communities or counseling, is vital for holistic recovery. This integrated approach ensures that patients feel supported and empowered throughout their healing journey, transforming potential distress into a manageable part of their transformation.
Ultimately, the long-term success of abdominoplasty hinges on a sustained commitment to self-care and ongoing vigilance. While most lumps resolve with time and appropriate intervention, maintaining a stable weight and healthy habits is crucial for preserving the aesthetic results and preventing future complications. The insights shared here are designed to empower you, the patient, with the knowledge and confidence to navigate every stage of your recovery. By understanding the ‘why’ and ‘how’ behind post-surgical lumps, you can actively participate in your healing, ensuring that your journey culminates in the desired outcome: a revitalized sense of self and a truly confident abdominal contour.
If you are experiencing any lumps or concerns after your abdominoplasty, remember that personalized medical advice is indispensable. Do not hesitate to consult with a board-certified plastic surgeon. Their expertise will provide you with an accurate diagnosis and a tailored treatment plan, guiding you towards the optimal recovery you deserve.
Frequently Asked Questions About Lumps After Abdominoplasty
When do lumps typically disappear after a tummy tuck?
The timeline for lumps to disappear varies depending on their cause. General swelling and minor irregularities usually subside within a few weeks to a few months. Seromas often resolve after aspiration, while scar tissue can take six to twelve months or longer to soften and flatten.
Can I prevent lumps after abdominoplasty?
While some lumpiness is a normal part of healing, you can minimize the risk by choosing an experienced, board-certified surgeon, diligently following all post-operative instructions (especially wearing compression garments), maintaining a healthy lifestyle, and avoiding smoking.
Is massage effective for post-tummy tuck lumps?
Yes, manual lymphatic drainage (MLD) massage, performed by a certified therapist, can be very effective for reducing fluid accumulation (seromas) and softening scar tissue. Always consult your surgeon before starting any massage regimen.
What if a lump is painful or growing?
If a lump is painful, rapidly growing, accompanied by redness, warmth, fever, or discharge, you should contact your plastic surgeon immediately. These could be signs of a complication like infection or a large hematoma requiring prompt medical attention.
Will lumps affect my final aesthetic result?
Many lumps are temporary and resolve with proper care, ultimately not affecting the final aesthetic outcome. However, persistent or untreated lumps, such as significant scar tissue or fat necrosis, could potentially impact the smoothness and contour of your abdomen. Early intervention is key to achieving the best possible result.
Bibliography
- American Society of Plastic Surgeons. (n.d.). Addominoplastica. Retrieved from https://www.plasticsurgery.org/cosmetic-procedures/tummy-tuck
- Mayo Clinic Staff. (2025, January 17). Addominoplastica. Mayo Clinic. Retrieved from https://www.mayoclinic.org/tests-procedures/tummy-tuck/about/pac-20384892
- Ruli. (2025, February 25). Troubleshooting Hard Lumps After Abdominoplasty Tips and Advice. Retrieved from https://en.ruli.com/article/troubleshooting-hard-lumps-after-abdominoplasty-tips-and-advice
- Ruli. (2025, February 12). Hard Lumps After Tummy Tuck Causes, Treatment, and Prevention. Retrieved from https://us.ruli.com/article/hard-lumps-after-tummy-tuck-causes-treatment-and-prevention
- Ruli. (2025, February 8). Preventing and Treating Hard Lump Formation after Abdominoplasty. Retrieved from https://us.ruli.com/article/preventing-and-treating-hard-lump-formation-after-abdominoplasty
- Tri Valley Plastic Surgery. (n.d.). Lumps Post-Tummy Tuck surgery. Retrieved from https://www.trivalleyplasticsurgery.com/resources/patient-questions/lumps-post-tummy-tuck-surgery/