As a surgeon specializing in aesthetic procedures, I frequently encounter patients seeking to enhance their silhouette and confidence through breast augmentation. This operation, formally known as augmentation mammoplasty, is one of the most commonly performed cosmetic surgeries globally, and for good reason. It offers a predictable and often profoundly satisfying way for individuals to achieve their desired breast volume, shape, and overall symmetry. Antalya, with its growing reputation as a hub for medical tourism, provides an environment where state-of-the-art medical facilities and experienced surgical teams converge, offering a compelling option for those considering this transformative procedure.
My approach to breast augmentation is rooted in a deep understanding of anatomy, aesthetic principles, and, critically, the unique aspirations of each patient. This is not a one-size-fits-all procedure; it is a highly individualized surgical endeavor requiring careful planning, meticulous execution, and comprehensive post-operative care. My aim is always to achieve results that are not only aesthetically pleasing and harmonious with the patient’s natural physique but also feel natural to the touch and stand the test of time.
In this extensive guide, I want to take you through the intricate journey of breast augmentation from my perspective as your potential surgeon. We will delve into the detailed considerations, the technical aspects, the recovery process, and the nuances that contribute to a successful outcome. My goal is to equip you with a thorough understanding of what the procedure entails, using precise medical terminology where necessary, but always providing clear, simple explanations to ensure you are fully informed every step of the way.
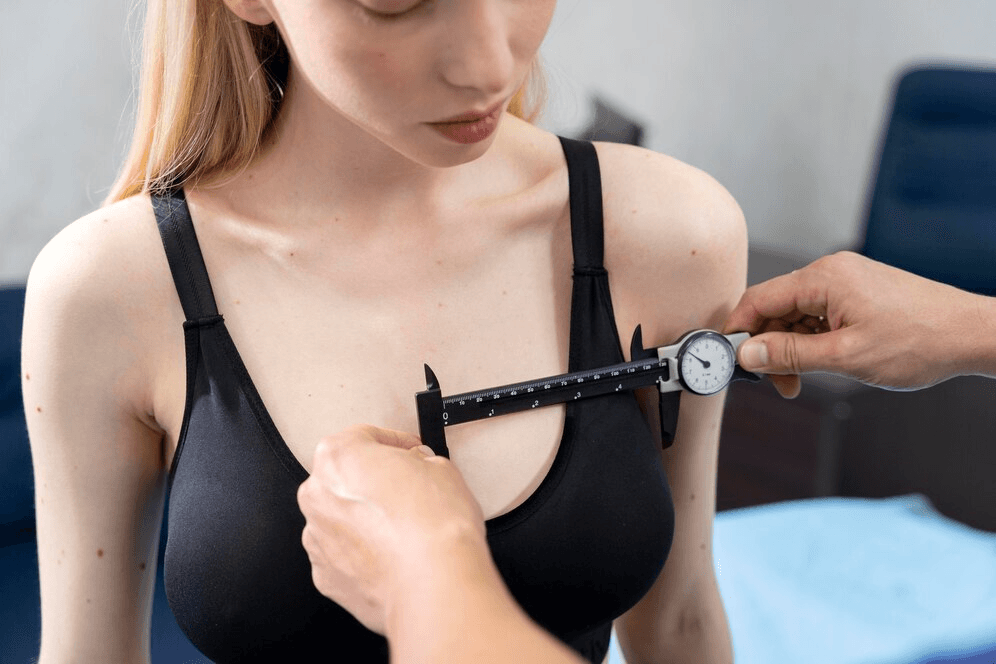
Table of Contents
The Initial Consultation: Laying the Foundation for Success
The journey towards achieving your desired breast size and shape begins long before you ever enter the operating theatre. It starts with the initial consultation. This is perhaps the most critical phase, a comprehensive discussion where I, as your surgeon, gain a deep understanding of your motivations, expectations, and medical history, while you gain insight into the possibilities and realities of the procedure.
Understanding Your Motivations and Goals
During this initial meeting, my primary focus is to listen. I need to understand why you are considering breast augmentation. Are you seeking to restore volume lost after pregnancy or weight loss? Do you wish to correct asymmetry between your breasts? Are you looking to enhance your overall body proportions? Your reasons are personal and important, and articulating them clearly helps me understand your aesthetic goals. We discuss the desired outcome in terms of size, shape, and projection. I encourage patients to bring photos that illustrate the look they admire, not necessarily to replicate them exactly, but to help translate subjective preferences into objective surgical goals.
The Anamnesis: Gathering Your Medical History
A crucial part of the consultation is taking a detailed anamnesis. This is the formal medical term for gathering your medical history. I will ask about past surgeries, existing medical conditions (such as diabetes, heart disease, or autoimmune disorders), allergies to medications, and current medications you are taking (including prescription drugs, over-the-counter medications, and supplements). Smoking status is particularly important, as smoking can significantly impair healing and increase the risk of complications. I will also inquire about your family history, particularly regarding breast cancer, as this may influence screening recommendations or surgical planning in the future. Understanding your overall health status is paramount to ensuring your safety and minimizing potential risks during and after surgery.
The Physical Examination: Assessing Your Anatomy
Following the discussion, a thorough physical examination is performed. This involves evaluating your chest wall anatomy, the existing size and shape of your breasts, the elasticity and quality of your skin, the position of your nipples, and the amount of existing breast tissue and subcutaneous fat. I will take precise measurements, including the width of your breast base, the distance from the sternal notch (the dip in your collarbone) to the nipple, and the amount of ptosis (sagging) present. These measurements are objective data points that, combined with your aesthetic goals and my surgical expertise, help inform the optimal implant size, shape, and placement. I also assess the tone and position of your pectoral muscles, as this influences whether the implant is best placed above or below the muscle.
Setting Realistic Expectations: The Art of the Possible
A significant part of the consultation is dedicated to managing expectations. While breast augmentation can achieve remarkable improvements, it’s essential to have a realistic understanding of what is surgically possible and how the results will integrate with your unique anatomy. We will discuss the concept of “profile” (how much the implant projects forward) and how different implant volumes and profiles will look on your frame. I may use sizing implants or computer simulations to give you a visual representation of potential outcomes. It’s important to understand that the final result is influenced by your existing anatomy, skin elasticity, and the healing process. My role is to guide you towards a choice that aligns with your desires while ensuring a natural and harmonious outcome.
Addressing Psychological Readiness
While primarily a physical transformation, breast augmentation also has a significant psychological component. I assess your psychological readiness and ensure you have a stable self-image and realistic expectations. Body dysmorphia, a condition where a person has an excessive preoccupation with a perceived flaw in their physical appearance, can sometimes be a contraindication for elective cosmetic surgery. It’s important that you are seeking surgery for yourself and have a healthy perspective on the potential changes.

Understanding Breast Anatomy in the Context of Augmentation
To truly appreciate the surgical process, it’s helpful to have a basic understanding of the relevant breast anatomy. From a surgical perspective, the breast is a complex structure composed of several layers, and the implant will be placed within a carefully created space, or “pocket,” relative to these layers.
The Chest Wall: The Foundation
Beneath the breast lies the chest wall, which consists of the ribs and the muscles that cover them. The most prominent muscle here is the pectoralis major muscle, a large, fan-shaped muscle that lies directly beneath the breast tissue. This muscle plays a crucial role in determining the implant placement option.
Breast Tissue: Glandular and Adipose Components
The breast itself is primarily composed of mammary gland tissue, responsible for milk production, and adipose tissue, which is fat. The proportion of glandular to adipose tissue varies among individuals and can change throughout life due to hormonal fluctuations, pregnancy, and weight changes. This composition influences the natural shape and density of the breast and affects how the implant will be supported and covered.
The Skin and Subcutaneous Tissue: The Envelope
The breast is enveloped by skin and subcutaneous tissue, which is the layer of fat and connective tissue directly beneath the skin. The elasticity and thickness of the skin are important factors. Good skin elasticity allows the skin to conform well to the new shape and volume provided by the implant. Thin or inelastic skin may be more prone to visible rippling of the implant, particularly with saline implants or in certain implant placements.
The Nipple-Areola Complex
The nipple-areola complex is the pigmented area surrounding the nipple. Its size, shape, and position are carefully considered during the pre-operative planning phase to ensure the final result looks balanced and natural. Incisions can sometimes be placed along the edge of the areola (periareolar incision), making the resulting scar less conspicuous.

Choosing Your Implants: Size, Shape, and Surface
One of the most significant decisions in breast augmentation is the choice of implants. This involves considering the filler material, the shape, and the surface texture.
Saline vs. Silicone Implants: The Filler
Historically, saline implants were widely used. These consist of a silicone elastomer shell filled with sterile saline solution during the surgical procedure. Saline implants have the advantage that they can be inserted through a smaller incision because they are filled after placement. However, they can feel less natural than silicone implants and there is a small risk of deflation over time, which is usually immediately noticeable.
Silicone implants are the most popular choice today. They are pre-filled with a cohesive silicone gel that mimics the feel of natural breast tissue. There are different levels of gel cohesiveness, ranging from very soft to form-stable (“gummy bear”) implants. Silicone implants typically require a slightly longer incision for insertion. While concerns about silicone leakage have been largely addressed with advanced manufacturing techniques and more cohesive gels, rupture can still occur, and it may not be immediately apparent (“silent rupture”), often requiring imaging like an MRI for detection. The feeling of silicone implants is generally considered more natural compared to saline.
Round vs. Anatomical Implants: The Shape
Implants come in two primary shapes: round and anatomical (often referred to as “teardrop” or “shaped” implants).
Round implants have a symmetrical shape and provide fullness primarily in the upper part of the breast, creating a rounder, more augmented look. They are less prone to rotation issues because their symmetry means that even if they spin within the pocket, the shape of the breast doesn’t change.
Anatomical implants are designed to mimic the natural slope of the breast, with more fullness at the bottom and tapering towards the top. They are often preferred for achieving a more naturalistic result, particularly in patients with minimal existing breast tissue or those seeking a subtle enhancement. However, due to their specific shape, rotation of an anatomical implant can distort the breast shape and may require revision surgery to correct. The shell of anatomical implants is usually textured to help them adhere to the surrounding tissue and minimize the risk of rotation.
Smooth vs. Textured Surfaces: The Shell
The outer shell of breast implants can be either smooth or textured.
Smooth implants have a soft, pliable shell that moves more freely within the tissue pocket. This can contribute to a more natural feel and drape of the breast. However, they may have a slightly higher risk of capsular contracture compared to textured implants.
Textured implants have a roughened surface. The idea behind texturing is that the surrounding tissue grows into the surface irregularities, helping to hold the implant in place and potentially reducing the incidence of capsular contracture. Different levels of texturing exist, from subtly textured to macro-textured. Concerns have been raised about a rare association between certain types of macro-textured implants and anaplastic large cell lymphoma (ALCL), a rare type of lymphoma. This has led to regulatory actions and a shift in surgical preference towards smooth or micro-textured implants in many regions. I will discuss the current understanding of ALCL and its association with implant texture during your consultation, ensuring you have the most up-to-date information to make an informed decision.
My recommendation for implant type, size, shape, and surface texture will be based on a careful assessment of your anatomy, your aesthetic goals, your lifestyle, and the latest medical evidence regarding safety and long-term outcomes.
Implant Placement: Above or Below the Muscle?
The positioning of the implant relative to the chest wall muscles is a critical decision that affects the final appearance, feel, and potential long-term outcomes of the augmentation. The two primary planes for implant placement are subglandular (above the muscle) and submuscular (below the muscle). A third technique, called the dual plane, combines aspects of both.
Subglandular Placement: Above the Muscle
Subglandular placement means the implant is placed directly beneath the existing breast tissue and above the pectoralis major muscle. This is a simpler dissection and may result in a quicker recovery with less initial pain. However, in patients with very little natural breast tissue, the edges of the implant may be more visible or palpable, creating a less natural look, particularly in the upper part of the breast. There might also be a slightly higher risk of capsular contracture in this plane compared to submuscular placement, although surgical technique and implant type also play significant roles. Mammographic screening for breast cancer can sometimes be more challenging with subglandular implants, as the implant can obscure some breast tissue; however, experienced radiologists are adept at using displacement techniques or supplementary imaging like ultrasound.
Submuscular Placement: Below the Muscle
Submuscular placement involves placing the implant, either partially or fully, beneath the pectoralis major muscle. This provides a layer of muscle tissue covering the upper part of the implant, which can help create a smoother, more natural transition from the chest wall to the breast, especially in patients with thin tissue coverage. This placement is often preferred when using saline implants to minimize visible rippling. Submuscular placement is associated with a lower incidence of capsular contracture compared to subglandular placement. However, the dissection required is more extensive, leading to more post-operative pain, swelling, and a longer initial recovery period. There is also a potential for animation deformity, where the breast distorts slightly when the pectoralis muscle is contracted, which can be a concern for athletes or those with highly developed chest muscles. Mammography is generally easier with submuscular implants as the muscle can be used to displace the implant away from the breast tissue.
Dual Plane Placement: A Hybrid Approach
The dual plane technique is a sophisticated approach that combines elements of both subglandular and submuscular placement. In this method, the upper part of the implant is placed beneath the pectoralis muscle, while the lower part is positioned beneath the breast tissue and the lower edge of the muscle is released. This technique aims to leverage the advantages of submuscular placement (better upper pole coverage, potentially lower capsular contracture risk) while allowing the lower part of the implant to sit more naturally and reduce the risk of upward migration. The dual plane technique is often favored for achieving a natural look with good projection, particularly in patients with mild to moderate ptosis. The complexity of the dissection and recovery profile falls somewhere between purely subglandular and purely submuscular placement.
The choice of implant placement is a crucial decision made during the consultation, tailored to your specific anatomy, the type and size of the implant chosen, and your desired aesthetic outcome. My recommendation will be based on extensive experience and a thorough understanding of the biomechanics and long-term implications of each placement option.
Incision Techniques: Minimizing Visible Scarring
The location of the surgical incision determines where the scar will be located. My aim is always to choose an incision site that allows for safe and efficient placement of the implant while resulting in the most inconspicuous scar possible. The most common incision techniques include the inframammary fold, periareolar, and transaxillary approaches. The transumbilical approach is less common for primary augmentation and is primarily used with saline implants.
Inframammary Fold Incision
The inframammary fold incision is the most common approach. The incision is made in the natural crease beneath the breast where the breast meets the chest wall. This location offers direct access to the breast pocket, allows for excellent visibility during surgery, and the resulting scar is typically well-hidden within the natural fold once the breast is augmented. This approach is versatile and can be used for both saline and silicone implants, regardless of placement plane.
Periareolar Incision
The periareolar incision is made along the edge of the areola, often following the transition line between the darker areolar skin and the lighter breast skin. This location allows the scar to blend with the color and texture changes of the areola, making it less noticeable. However, this approach may not be suitable for patients with very small areolas, and there is a slightly higher theoretical risk of impacting nipple sensation or milk ducts compared to the inframammary approach, although in skilled hands, this risk is low.
Transaxillary Incision
The transaxillary incision is made in the armpit (axilla). The implant is then inserted through a tunnel created from the armpit to the breast pocket. This technique leaves no scar on the breast itself, which is appealing to many patients. However, it is a more indirect approach, which can make precise pocket creation and implant positioning slightly more challenging, particularly with anatomical implants. There is also a theoretical risk of nerve damage in the armpit, although this is rare.
Transumbilical Breast Augmentation (TUBA)
Transumbilical breast augmentation (TUBA) involves making an incision around the belly button (umbilicus) and creating a tunnel up to the breast pocket. This technique is primarily used for saline implants, which are filled after being guided into the pocket. While it leaves no scar on the breast or armpit, it is a more technically challenging procedure with limited control over pocket dissection and implant positioning compared to other approaches. Consequently, it is less commonly performed for primary augmentation.
The choice of incision will be made in consultation with you, considering your anatomy, implant type and placement, and your preferences regarding scar location. My priority is to ensure a safe and effective procedure with the best possible aesthetic outcome.
The Surgical Procedure: A Meticulous Process
Once the pre-operative planning is complete and we have agreed on the implant type, size, placement, and incision technique, we proceed to the surgical phase. Breast augmentation is typically performed as an outpatient procedure, meaning you can go home the same day, although some patients may require an overnight stay for monitoring.1
Pre-operative Preparation and Anesthesia
On the day of surgery, you will meet with the surgical team, including the anesthesiologist. The anesthesiologist will discuss the type of anesthesia that will be used. Breast augmentation is most commonly performed under general anesthesia, where you are completely asleep and unaware during the procedure. In some cases, it may be performed under local anesthesia with sedation, where the breast area is numbed, and you are given medication to relax and make you drowsy. The choice of anesthesia depends on the complexity of the procedure, your health status, and your preferences. Throughout the surgery, your vital signs (heart rate, blood pressure, oxygen levels) will be closely monitored by the anesthesiologist and the surgical nurse.
Before the anesthesia is administered, I will make pre-operative markings on your chest while you are standing. These markings guide the incision and pocket creation and ensure symmetry. This is a critical step, as positioning yourself while standing allows for accurate marking based on gravity and your natural posture.
Creating the Implant Pocket
Once the anesthesia has taken effect and the surgical area has been prepared using aseptic technique (meaning sterile procedures to prevent infection), I will make the planned incision. Using specialized surgical instruments, I will then carefully create a pocket to accommodate the implant. The size and location of this pocket are meticulously dissected to match the dimensions of the chosen implant and the planned placement plane (subglandular, submuscular, or dual plane). Dissection is the process of separating tissue layers. Throughout this process, hemostasis (controlling bleeding) is paramount to minimize bruising and the risk of hematoma formation. I use electrocautery or other techniques to seal small blood vessels as I proceed.
Inserting the Implant
With the pocket created, the implant is carefully inserted. If using saline implants, the empty shell is placed, and then sterile saline solution is injected through a valve to inflate it to the desired volume. With silicone implants, the pre-filled implant is guided into the pocket. Sterile technique is critical during this phase to prevent contamination of the implant. I often use a funnel-like device to help insert silicone implants with minimal contact, further reducing the risk of infection.
Closure and Dressings
Once the implant is correctly positioned and its symmetry checked, the incision is closed in layers using sutures. I use dissolvable sutures for the deeper layers and often fine sutures or surgical glue for the skin closure to minimize scarring. Suturing is the process of stitching tissue together. A sterile dressing is applied, and a compression garment or surgical bra is usually placed to provide support and help reduce swelling and bruising. In some cases, a temporary drain may be inserted to help remove any excess fluid that may accumulate in the pocket; this is more common with submuscular placement. The drain is typically removed within a few days.
Anesthesia and Patient Safety: A Top Priority
Patient safety is the cornerstone of my practice. The involvement of a qualified anesthesiologist and a skilled surgical team is non-negotiable.
Types of Anesthesia
As mentioned, general anesthesia is most common. This renders you unconscious and pain-free throughout the procedure. The anesthesiologist carefully monitors your vital signs and manages your airway and breathing. Local anesthesia with sedation is an option for some patients and procedures, where the surgical area is numbed with a local anesthetic, and you receive intravenous medication to relax you. You remain conscious but are typically drowsy and comfortable. The choice depends on the planned surgery’s extent, your health, and the anesthesiologist’s assessment.
Monitoring During Surgery
Throughout the operation, the anesthesiologist continuously monitors your heart rate, blood pressure, oxygen saturation, carbon dioxide levels, and temperature. This vigilance allows for immediate detection and management of any physiological changes.
The Surgical Team
Beyond the surgeon and anesthesiologist, the surgical team includes experienced surgical nurses and scrub technologists. The surgical nurse assists the anesthesiologist and monitors the patient’s overall condition. The scrub technologist prepares the sterile instruments and hands them to the surgeon during the procedure. This coordinated team effort is essential for a smooth and safe operation.
Protocols for Patient Safety
My practice adheres to stringent safety protocols, including pre-operative checklists, verification of patient identity and planned procedure, and meticulous sterile techniques. We also have protocols in place for managing potential complications, although fortunately, they are rare. Your safety is my utmost concern throughout the entire surgical process.
Recovery and Post-Operative Care: Navigating the Healing Process
The surgical procedure is only one part of the journey; the recovery period is equally important for achieving a successful outcome and ensuring a smooth healing process. My team and I provide detailed instructions and support to guide you through this phase.
Immediate Post-Operative Period
Immediately after surgery, you will be taken to a recovery room where you will be monitored as you wake up from anesthesia. It is normal to feel groggy, and you may experience some pain, discomfort, and swelling in the chest area. Post-operative analgesia (pain relief medication) will be administered to manage your discomfort. Nausea can sometimes occur as a side effect of anesthesia, and medication can be given to alleviate this.
Pain Management
Pain levels vary among patients and depending on the implant placement (submuscular placement typically involves more initial pain). You will be prescribed pain medication to take at home. It’s important to take this medication as directed to stay comfortable. Most significant pain subsides within the first few days, transitioning to soreness and tightness over the following weeks.
Swelling and Bruising
Swelling and bruising are normal after breast augmentation. Applying cold compresses as directed can help reduce swelling. Wearing the provided compression garment or surgical bra is essential during the initial recovery period. This garment provides support, helps reduce swelling, and helps the tissues conform to the new shape. Swelling typically peaks within the first 72 hours and gradually subsides over the following weeks and months. Bruising may spread downwards due to gravity but will eventually resolve.
Activity Restrictions
You will have activity restrictions during the initial recovery period. Heavy lifting, strenuous exercise, and activities that involve significant arm or chest movement should be avoided for several weeks. You will be advised to sleep on your back to avoid putting pressure on your breasts. Gradual return to normal activities will be permitted based on your healing progress. I will provide a detailed timeline for when you can resume specific activities.
Follow-Up Appointments
Scheduled follow-up appointments are crucial. During these visits, I will monitor your healing, check the incisions, assess for any signs of complications such as seroma (fluid collection) or hematoma (blood collection), and answer any questions you may have. Drainage tubes, if placed, will be removed during a follow-up visit. These appointments allow me to ensure you are healing appropriately and to address any concerns promptly.
Managing Incision Care
You will receive specific instructions on how to care for your incisions. This typically involves keeping them clean and dry and applying any prescribed ointments. Itching around the incisions is common as they heal. It’s important not to pick at the scabs and to protect the scars from sun exposure for at least a year, as sunlight can cause them to darken and become more noticeable.
The Healing Timeline
The healing process is a gradual one. While the initial recovery takes a few weeks, it can take several months for all the swelling to subside, for the implants to settle into their final position, and for the scars to mature and fade. Sensation in the nipples and breast skin may be altered temporarily, feeling numb or overly sensitive. This usually resolves over time, although in rare cases, changes in sensation can be permanent.
Potential Risks and Complications: Transparency and Preparedness
While breast augmentation is generally a safe procedure when performed by a qualified surgeon, it is still surgery and carries potential risks and complications. A thorough discussion of these possibilities is an essential part of the informed consent process. It’s important to understand that while complications can occur, their incidence is relatively low, and in most cases, they can be successfully managed.
Capsular Contracture: The Scar Tissue Tightening
One of the most common complications is capsular contracture. The body naturally forms a fibrous capsule of scar tissue around any foreign object, including a breast implant. In some cases, this capsule can tighten and constrict around the implant, causing the breast to become hard, painful, and distorted in shape. The exact cause of capsular contracture is not fully understood, but factors such as infection, hematoma, and genetics may play a role. It is graded on a scale from I (soft breast) to IV (hard, painful, and distorted). Mild contracture (Grade I-II) may not require intervention, but more severe contracture (Grade III-IV) typically requires revision surgery to remove or release the tightened capsule (capsulectomy or capsulotomy) and potentially replace the implant. The risk of capsular contracture is generally lower with submuscular placement and textured implants (though the latter has other considerations).
Infection: A Serious Concern
Like any surgery, there is a risk of infection. An infection around a breast implant is a serious complication that usually requires removal of the implant, a course of antibiotics, and potentially a period of waiting before a new implant can be placed. Strict sterile technique during surgery and proper post-operative care help minimize this risk. Signs of infection include increased pain, redness, swelling, warmth, and fever. Prompt medical attention is crucial if you suspect an infection.
Hematoma and Seroma: Fluid Collections
Hematoma is a collection of blood outside of a blood vessel, essentially a large bruise. Seroma is a collection of clear fluid. Small hematomas and seromas may resolve on their own, but larger collections may require drainage with a needle or, in some cases, a return to the operating room to stop the bleeding and remove the clot or fluid. Drains are sometimes used initially to help prevent the accumulation of seroma.
Implant Rupture or Deflation
While modern implants are durable, they are not designed to last a lifetime and can rupture or deflate. Saline implant deflation is usually immediately noticeable as a sudden decrease in breast size. The saline solution is safely absorbed by the body. Silicone implant rupture may be silent (asymptomatic) and not immediately apparent. Silicone gel is cohesive and typically remains within the fibrous capsule, but it can spread over time if the rupture is not addressed. Routine monitoring with imaging (ultrasound or MRI) is recommended for silicone implants to detect silent ruptures. Implant rupture typically requires revision surgery to remove the ruptured implant and replace it.
Rippling and Folding
In some cases, the edges or folds of the implant may become visible or palpable through the skin, particularly in patients with thin tissue coverage or if saline implants are used. This is known as rippling or folding. It is often more noticeable in the subglandular plane. Choosing the appropriate implant size and placement based on your tissue thickness can help minimize this risk.
Implant Malposition
Implant malposition occurs when the implant shifts from its intended position. This can be due to insufficient pocket dissection, capsular contracture, or trauma. It can result in the breasts looking asymmetrical or unnatural. Correction typically requires revision surgery to reposition the implant and potentially modify the pocket.
Delayed Wound Healing
While most incisions heal well, factors like smoking, poor nutrition, or underlying medical conditions can impair wound healing, leading to delayed closure or increased risk of infection.
Changes in Nipple or Breast Sensation
Temporary changes in sensation are common after breast augmentation, ranging from numbness to increased sensitivity. In most cases, sensation returns to normal over time, but permanent changes, including complete loss of sensation, are possible, though rare.
Anaplastic Large Cell Lymphoma (ALCL)
As mentioned earlier, there is a rare association between certain types of textured breast implants and Breast Implant-Associated Anaplastic Large Cell Lymphoma (BIA-ALCL). This is not a cancer of the breast tissue itself but a rare type of lymphoma that can develop in the fluid or scar capsule around the implant. The risk is considered very low, particularly with smooth or micro-textured implants, which are the predominant types used today. Symptoms typically include late-onset seroma, swelling, or a mass. BIA-ALCL is generally curable with surgical removal of the implant and capsule. I stay informed about the latest research and regulatory updates regarding BIA-ALCL and discuss this with you during the consultation.
My responsibility is to fully inform you of these potential risks and complications. We will discuss their likelihood based on your individual circumstances and the choices we make regarding the surgical plan. Informed consent means you have a clear understanding of the potential benefits and risks before proceeding with surgery.
Managing Expectations and Achieving Natural Results: The Art and Science
Breast augmentation is as much an art as it is a science. My goal is not just to increase breast size but to create breasts that look and feel natural and are in proportion with your body. Achieving a truly aesthetic result involves carefully balancing your desires with the realities of your anatomy and the capabilities of the surgical techniques.
The Importance of Proportion
Choosing the right implant size and shape is crucial for achieving a natural look. Implants that are too large for your chest width or tissue coverage can look unnatural, increase the risk of complications like rippling or malposition, and may not feel comfortable. We use measurements and potentially sizing implants during the consultation to help visualize how different volumes will look on your frame. My experience guides the selection of an implant that will provide the desired enhancement while maintaining harmonious proportions with your shoulders, hips, and overall physique.
Understanding “Natural Feel”
The “natural feel” of augmented breasts is influenced by several factors: the type of implant (silicone generally feels more like natural tissue than saline), the amount of your own breast tissue covering the implant, and the implant placement (submuscular placement often provides better coverage and a softer feel in the upper pole). While augmented breasts will feel different from non-augmented breasts, particularly to deep palpation, the goal is for them to feel soft and natural to the touch in daily life.
The Role of Existing Anatomy
Your existing breast shape, skin elasticity, and the amount of natural breast tissue all play a significant role in the final outcome. Patients with more natural tissue tend to achieve a softer, more natural look with less visibility of the implant edges. Skin elasticity affects how well the skin conforms to the new shape; poor elasticity can sometimes limit the degree of augmentation that can be achieved naturally.
The Surgeon’s Aesthetic Judgment
Beyond the technical aspects, a surgeon’s aesthetic judgment is paramount. This involves understanding what constitutes a balanced and aesthetically pleasing breast shape in relation to the individual patient’s body. It’s about creating a smooth transition from the chest wall, a pleasing cleavage, and a natural-looking profile. This is where experience and a keen eye for aesthetics come into play.
Long-Term Outcomes and Monitoring: A Lifelong Commitment
Breast implants are not lifetime devices. While modern implants are designed for durability, they can eventually wear out or rupture and may require replacement or removal at some point in the future. Understanding the long-term considerations and the importance of ongoing monitoring is crucial.
Implant Longevity
The lifespan of a breast implant varies. Some implants may last for decades, while others may require replacement sooner due to rupture, capsular contracture, or simply a desire for a change in size or shape. It’s important to view breast augmentation as a procedure that may require future surgical intervention.
Routine Monitoring
Routine monitoring is recommended for all patients with breast implants. For silicone implants, this typically includes a baseline MRI scan a few years after surgery and subsequent scans every few years thereafter to check for silent rupture, as recommended by regulatory bodies. Physical examinations during your annual check-ups with your plastic surgeon are also important to assess the implants and the surrounding tissues.
Mammography and Other Imaging
Breast implants can sometimes make it more challenging to detect breast cancer on standard mammograms. It is essential to inform the mammography technician that you have implants. Experienced technologists use special displacement techniques to visualize as much breast tissue as possible. In some cases, supplementary imaging, such as ultrasound or MRI, may be recommended to get a clearer view of the breast tissue. It’s important to continue with your regular breast cancer screening as recommended by your physician.
Revision Surgery
Revision surgery refers to any subsequent surgery performed on breasts that have previously undergone augmentation. Reasons for revision surgery can include capsular contracture, implant rupture or deflation, malposition, desired change in size or shape, or aesthetic concerns. Revision surgery is often more complex than the initial augmentation, as it involves working in tissue that has already been surgically altered and has scar tissue. The complexity and recovery vary depending on the reason for the revision.
My commitment to you extends beyond the initial surgery. I am here to provide long-term care and guidance, monitoring your implants and addressing any concerns that may arise over time.
Antalya: A Considered Choice for Medical Tourism
Antalya has emerged as a significant destination for medical tourism, attracting patients from around the world seeking high-quality medical care in a desirable location. While my primary focus as a surgeon is on providing exceptional surgical care, I understand the appeal of undergoing surgery in a place like Antalya.
State-of-the-Art Facilities
Antalya boasts modern hospitals and clinics equipped with advanced technology and adhering to international standards of safety and care. These facilities are designed to provide a comfortable and secure environment for surgical procedures and recovery.
Experienced Surgical Teams
The region is home to a number of highly qualified and experienced plastic surgeons, many of whom have trained internationally and specialize in cosmetic procedures like breast augmentation. My commitment to continuous learning and staying abreast of the latest surgical techniques and technologies ensures that I provide care that is both advanced and safe.
The Appeal of Recovery
Recovering from surgery requires rest and a supportive environment. Antalya offers a pleasant climate and relaxing surroundings, which can contribute to a more comfortable and less stressful recovery period. While it is important to prioritize rest and follow post-operative instructions meticulously, the ability to recover in a different environment can be appealing to many patients.
Choosing to have surgery in a foreign country requires careful consideration and thorough research. It is essential to select a reputable surgeon and facility, understand the logistics of travel and accommodation, and ensure you have adequate support during your recovery both locally and upon your return home. My team is available to help facilitate aspects of your journey, but the ultimate responsibility for research and preparation lies with the patient.
Frequently Asked Questions from a Surgeon’s Perspective
During consultations, certain questions arise frequently. Here are some of them, addressed from my viewpoint as your surgeon:
How painful is the recovery?
Pain is subjective and varies from person to person. The most intense pain is typically experienced in the first few days after surgery, especially with submuscular placement due to muscle dissection. However, this pain is manageable with prescribed pain medication. Discomfort, tightness, and soreness are more common sensations after the initial pain subsides. Most patients find the discomfort manageable within a week or two.
How long does it take to recover?
The initial recovery period, where you need significant rest and assistance, is typically 1-2 weeks. During this time, you will experience swelling, bruising, and limited mobility. You can usually return to light, sedentary work within 1-2 weeks. Strenuous activities and heavy lifting are restricted for at least 4-6 weeks. Full recovery, with all swelling subsided and implants settled, can take several months.
When can I return to exercise?
Light walking is encouraged soon after surgery to promote circulation. However, strenuous exercise, particularly activities that involve the chest muscles or bouncing, should be avoided for at least 4-6 weeks, or until cleared by me. We will discuss a gradual return to your exercise routine based on your healing.
Will I be able to breastfeed after breast augmentation?
In most cases, breast augmentation does not interfere with the ability to breastfeed. The mammary glands and milk ducts are generally not significantly disrupted by implant placement, particularly with inframammary or transaxillary incisions. However, the periareolar incision carries a slightly higher theoretical risk of impacting milk ducts. If future breastfeeding is a priority for you, please discuss this with me during the consultation so we can choose the most appropriate surgical approach.
Will breast implants make it harder to detect breast cancer?
As mentioned earlier, breast implants can sometimes make mammography slightly more challenging. However, it does not prevent the detection of breast cancer. It is crucial to inform the mammography technician about your implants so they can use appropriate techniques. Regular self-examinations and clinical breast exams by your doctor remain important screening methods. Supplemental imaging like ultrasound or MRI can be used if necessary.
Conclusion: A Journey Towards Confidence and Self-Esteem
Breast augmentation surgery is a significant decision and a journey that requires careful consideration, realistic expectations, and a partnership between you and your surgeon. My role is to guide you through this process, providing expertise, support, and personalized care every step of the way.
Achieving your desired breast size and shape can have a profound positive impact on your self-image, confidence, and overall well-being. Whether you are seeking to restore volume, correct asymmetry, or enhance your contours, breast augmentation can be a transformative procedure.
In Antalya, you have access to excellent medical facilities and experienced surgeons dedicated to providing high-quality care. By understanding the intricacies of the procedure, the recovery process, and the potential long-term considerations, you can make an informed decision that is right for you.
My commitment is to ensure your safety, minimize risks, and strive to achieve a result that is not only aesthetically pleasing and natural but also enhances your quality of life. If you are considering breast augmentation in Antalya, I invite you to schedule a consultation to discuss your goals and explore how this procedure can help you achieve the confidence and silhouette you desire.
Transform Your Confidence with Surgyteam!
Join the thousands of satisfied patients who have experienced the exceptional care and expertise of Surgyteam’s renowned plastic surgeons. Whether you’re seeking aesthetic enhancements or reconstructive surgery, our dedicated team in Antalya is here to provide you with the highest quality treatment and personalized care.


