Abdominoplasty, commonly known as a tummy tuck, is a significant surgical procedure aimed at removing excess skin and fat from the abdomen, tightening underlying muscles, and improving the overall contour of the midsection. While highly effective, access to this procedure within the National Health Service (NHS) is strictly controlled due to resource limitations and prioritization of urgent cases. This article outlines the key considerations regarding NHS eligibility for abdominoplasty.

Table of Contents
NHS Eligibility Criteria for Abdominoplasty
The NHS prioritizes surgical procedures based on clinical need, not cosmetic preference. Abdominoplasty is generally considered a cosmetic procedure unless it addresses a significant medical issue. Therefore, eligibility hinges on demonstrating a demonstrable medical necessity. This might include cases of diastasis recti (separation of abdominal muscles) causing significant discomfort or functional impairment, or excess skin resulting from massive weight loss that leads to skin infections, chronic sores, or significant physical limitations. The presence of hernias requiring repair in conjunction with the abdominoplasty might also enhance eligibility. In short, the procedure must address a clinically significant problem, not simply improve aesthetic appearance.
Eligibility is not guaranteed even with a medical need. Patients must meet specific health criteria, including a stable weight for at least six months prior to application, absence of significant smoking history (which compromises healing), and overall good general health. Pre-existing conditions such as diabetes, heart disease, or clotting disorders will be carefully evaluated to assess surgical risk. A thorough medical history and physical examination are mandatory. Patients with unrealistic expectations or poor understanding of the procedure and recovery process may be deemed unsuitable.
The application process involves a referral from a General Practitioner (GP) to a specialist plastic surgeon within the NHS. This referral must clearly articulate the medical necessity for the surgery, supported by detailed clinical documentation. The surgeon will then assess the patient’s suitability based on the criteria outlined above. The decision-making process is rigorous and considers both the potential benefits and risks of the procedure relative to the patient’s overall health. Patients should be prepared for a potentially lengthy assessment period.
Denial of funding is not uncommon. Many individuals seeking abdominoplasty on the NHS are ultimately unsuccessful due to a lack of demonstrable medical need. The NHS is obligated to allocate resources to procedures with the highest clinical priority, and abdominoplasty often falls outside this category unless exceptional circumstances exist. Transparency regarding the decision-making process is crucial, and patients should receive clear explanations for any denials.

Assessment and Prioritisation Process
Following GP referral, the patient will undergo a comprehensive assessment by a consultant plastic surgeon specializing in abdominoplasty. This assessment will involve a detailed medical history review, physical examination, and discussion of the patient’s expectations. Imaging studies, such as ultrasound or CT scans, may be necessary to evaluate the extent of diastasis recti or identify other underlying conditions. The surgeon will meticulously document the patient’s medical condition and the rationale for considering abdominoplasty.
The assessment also involves a thorough evaluation of the patient’s lifestyle and commitment to post-operative care. Factors such as smoking habits, diet, and physical activity level are crucial for successful healing and outcome. Patients must demonstrate a realistic understanding of the surgical procedure, potential complications, and the commitment required for recovery. Patients who fail to meet these expectations may be deemed unsuitable for surgery even if they meet the initial medical criteria.
Prioritization within the NHS is complex and involves a multi-faceted assessment. The severity of the medical condition necessitating the surgery, the potential impact on the patient’s quality of life, and the availability of NHS resources all play a role. Waiting lists for elective procedures like abdominoplasty can be extensive, and the precise waiting time is unpredictable. Patients should be prepared for a prolonged waiting period, potentially spanning several months or even years.
The decision regarding whether to proceed with the surgery rests ultimately with the NHS trust. The surgeon’s recommendation is a crucial factor, but it is not the sole determining factor. The final decision considers the overall demands on NHS resources and the relative urgency of other patients’ needs. While transparency is important, the decision-making process is often complex and may not be fully transparent to the patient.

Surgical Considerations and Alternatives
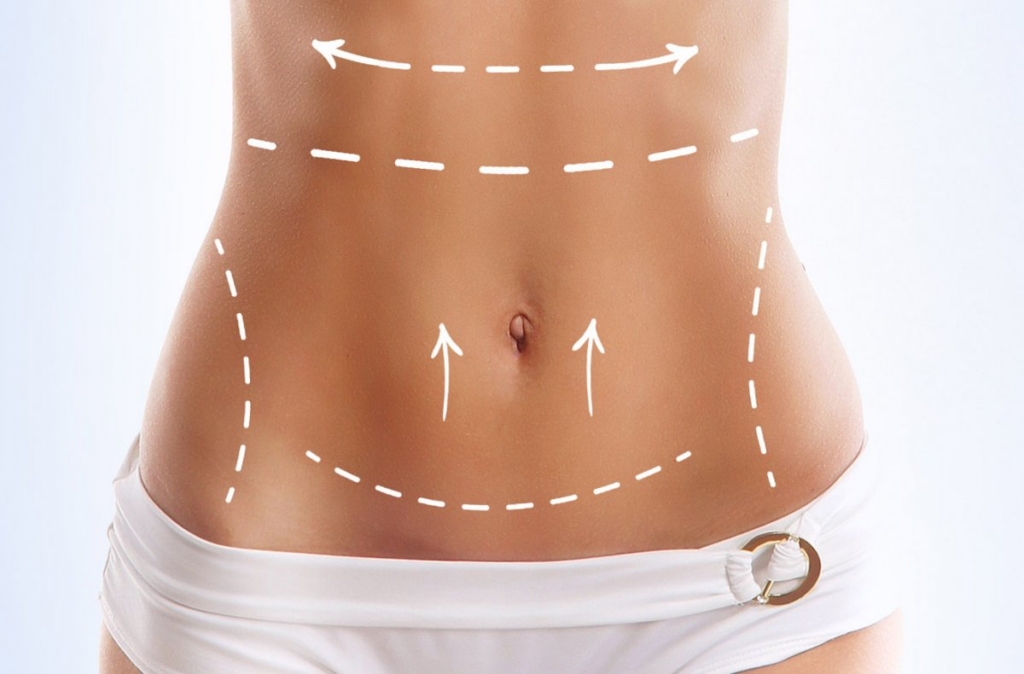
If deemed eligible for NHS-funded abdominoplasty, the surgical procedure itself will be performed by a qualified NHS consultant plastic surgeon. The specific surgical technique will be tailored to the individual patient’s anatomy and needs. The procedure typically involves removing excess skin and fat, tightening the abdominal muscles, and repositioning the umbilicus (belly button). The extent of the surgery will depend on the patient’s individual circumstances.
Alternatives to abdominoplasty should be discussed during the assessment process. These might include less invasive procedures such as liposuction, which targets fat removal but doesn’t address loose skin or muscle laxity. For diastasis recti, non-surgical approaches like physiotherapy and targeted exercises may be considered, especially in milder cases. The surgeon will explain the benefits and limitations of each option, helping the patient make an informed decision aligned with their individual needs and circumstances.
The NHS may not fund abdominoplasty if less invasive alternatives are deemed sufficient to address the underlying medical condition. For instance, if diastasis recti is mild and responds well to physiotherapy, abdominoplasty might be deemed unnecessary. The decision to pursue a less invasive approach is made collaboratively between the patient and the surgeon, considering both clinical effectiveness and resource allocation within the NHS.
The potential risks and complications of abdominoplasty must be fully understood. These include bleeding, infection, seroma formation (fluid accumulation), delayed wound healing, and changes in skin sensation. Rare but serious complications, such as blood clots or pulmonary embolism, are also possible. The surgeon will thoroughly discuss these risks during the pre-operative consultation, ensuring the patient is fully informed before proceeding.

Post-Operative Care and Recovery
Post-operative care following NHS abdominoplasty involves a combination of hospital stay (duration varies), outpatient appointments, and at-home recovery. Pain management is crucial, and the patient will receive prescriptions for pain medication. A compression garment is typically worn for several weeks to minimize swelling and support healing. Regular wound care is essential to prevent infection. Follow-up appointments with the surgical team are scheduled to monitor healing progress and address any complications.
Recovery from abdominoplasty is gradual and can take several months. Patients should expect significant discomfort and swelling in the initial weeks. Gradual return to normal activity is advised, with restrictions on strenuous physical activity for several weeks or months. The surgeon will provide specific guidance on activity levels and post-operative care instructions. Patients should adhere strictly to these instructions to optimize healing and minimize complications.
The NHS provides support during the recovery period, including access to physiotherapy, if needed. This support aims to facilitate optimal healing and rehabilitation. Patients should actively participate in their recovery by following prescribed exercises and attending all scheduled appointments. Open communication with the surgical team is vital to address any concerns or complications that may arise during recovery.
Long-term outcomes following abdominoplasty are generally positive, provided the patient adheres to post-operative instructions and maintains a healthy lifestyle. However, individual results may vary. The NHS will provide ongoing support as needed, but patients should be aware that complete healing and return to normal activity may take several months, and some degree of scarring is inevitable.
Securing NHS funding for abdominoplasty requires a demonstrable medical necessity beyond simple cosmetic enhancement. The assessment process is rigorous, and eligibility is not guaranteed. Understanding the eligibility criteria, assessment process, surgical considerations, and post-operative care is crucial for patients considering this procedure within the NHS framework. Alternatives to abdominoplasty should be discussed, and patients must be realistic about the potential challenges and limitations associated with accessing this procedure through the NHS.
Transform Your Confidence with Surgyteam!
Join the thousands of satisfied patients who have experienced the exceptional care and expertise of Surgyteam’s renowned plastic surgeons. Whether you’re seeking aesthetic enhancements or reconstructive surgery, our dedicated team in Antalya is here to provide you with the highest quality treatment and personalized care.