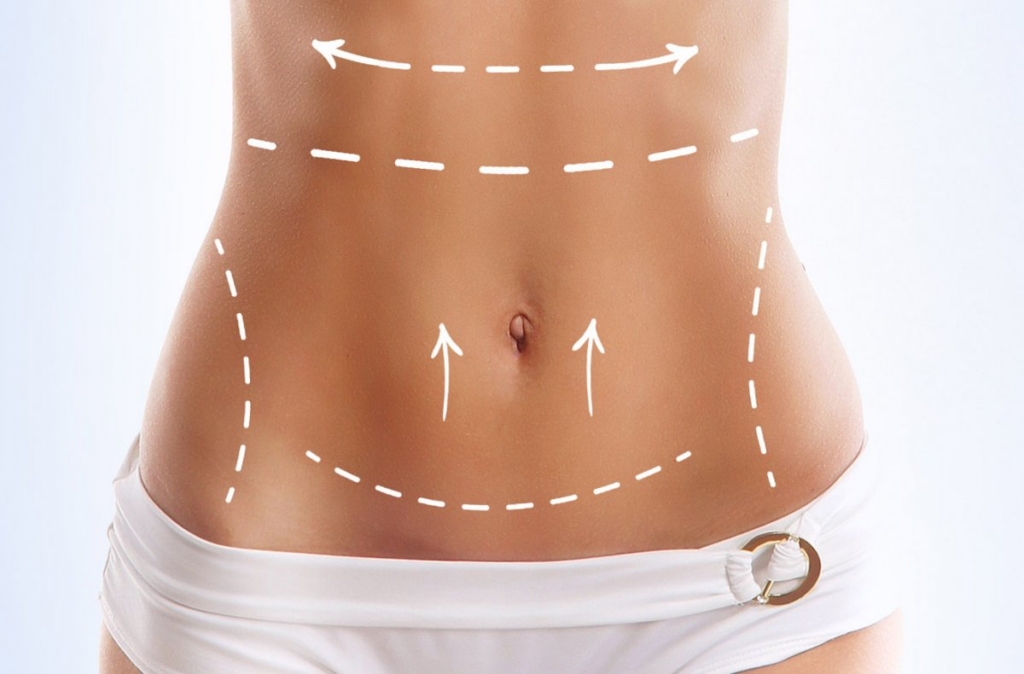
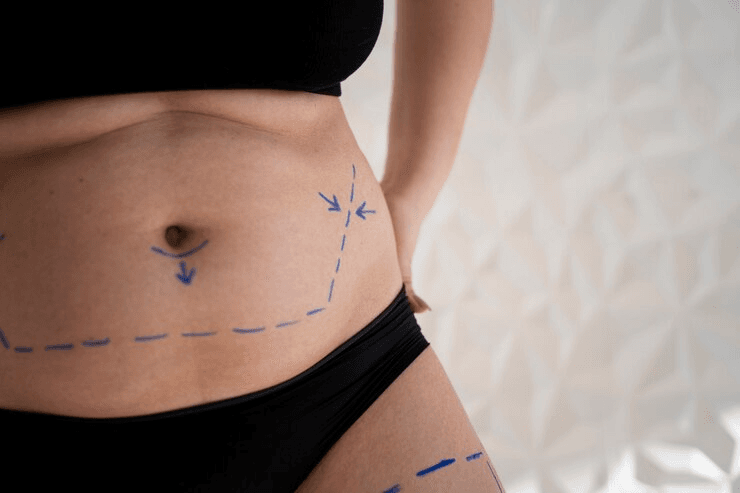
A tummy tuck, or abdominoplasty, aims to remove excess skin and fat, tighten abdominal muscles, and create a flatter, more toned abdomen. However, some patients experience persistent bulges or irregularities post-surgery. This is not uncommon and often resolves with time, but understanding the potential causes is crucial for managing expectations and addressing concerns. This article outlines several reasons why a bulge might persist after a tummy tuck.
Table of Contents
Understanding Post-Tummy Tuck Swelling
Post-operative swelling is a completely normal and expected phenomenon following an abdominoplasty. Significant fluid accumulation is common in the treated area, leading to a noticeable bulge. This swelling can be quite substantial initially and gradually diminishes over several weeks, even months. The degree of swelling varies significantly between patients, depending on factors such as individual healing response, surgical technique, and the extent of the procedure. Patience is key; the body requires time to reabsorb this excess fluid.
The location and distribution of swelling can also be informative. Generalized swelling across the abdomen is typical, but localized areas of greater prominence might indicate specific underlying issues, warranting further investigation. Compression garments, prescribed by your surgeon, are crucial in managing post-operative swelling by providing support and promoting lymphatic drainage. Regular follow-up appointments allow your surgeon to monitor progress and address any concerns.
Ignoring the prescribed post-operative care can significantly prolong the swelling phase and increase the risk of complications. This includes neglecting compression garment wear, failing to attend follow-up appointments, and engaging in strenuous activity prematurely. Adequate rest and a balanced diet also play a vital role in optimizing the healing process and minimizing prolonged swelling.
Failure to address underlying medical conditions, such as lymphatic dysfunction, can exacerbate post-operative swelling. Pre-operative assessment and management of such conditions are crucial for achieving optimal outcomes. Open communication with your surgeon is essential to ensure that any concerns regarding persistent swelling are addressed promptly and effectively.

Seromas and Fluid Collections
Seromas are collections of serous fluid that can accumulate beneath the skin following surgery. These fluid pockets can manifest as palpable bulges, mimicking the appearance of persistent fat or muscle laxity. Seromas are often asymptomatic but can become infected if left untreated. Diagnosis typically involves physical examination and, in some cases, ultrasound imaging.
Treatment of seromas may involve aspiration, a minimally invasive procedure where the fluid is removed using a needle. In some instances, a small incision might be necessary to facilitate drainage. The risk of seroma formation is influenced by several factors, including the extent of the surgery, the patient’s individual healing characteristics, and the surgical technique employed.
The size and location of a seroma can significantly impact its clinical significance. Small, asymptomatic seromas often resolve spontaneously, while larger collections may require intervention to prevent infection or discomfort. Prompt identification and management of seromas are crucial to prevent complications and ensure optimal aesthetic outcomes.
Prevention strategies, such as meticulous surgical technique and the use of drains, can help minimize the risk of seroma formation. However, despite the best efforts, seromas can still occur. Patients should be aware of the possibility of seroma formation and promptly report any new or worsening bulges to their surgeon.
Muscle Separation and Diastasis Recti
Diastasis recti, the separation of the rectus abdominis muscles, is a common condition, often exacerbated by pregnancy or significant weight fluctuations. While a tummy tuck aims to repair this separation, incomplete correction or recurrence can lead to a persistent bulge in the midline of the abdomen. This bulge is often most noticeable when the abdominal muscles are contracted, such as during coughing or straining.
Physical examination, often coupled with imaging techniques like ultrasound, can confirm the diagnosis of diastasis recti. The degree of separation is crucial in determining the appropriate management strategy. In some cases, conservative measures such as physical therapy focused on core strengthening may suffice.
For more significant separations, surgical revision may be necessary to achieve optimal aesthetic and functional results. This revision may involve re-approximation of the separated muscles, potentially requiring additional incisions or adjustments to the original tummy tuck. The decision regarding the need for revision is made on a case-by-case basis, considering the extent of diastasis and the patient’s goals.
Prevention of diastasis recti post-tummy tuck involves careful surgical planning and execution, along with adherence to post-operative instructions, including appropriate core strengthening exercises. Patients with pre-existing diastasis recti should discuss their concerns with their surgeon pre-operatively to manage expectations and explore potential solutions.

Skin Redundancy and Scar Tissue
Even with the removal of excess skin, some residual skin redundancy can remain, particularly in patients with significant weight loss or laxity. This can manifest as a subtle or more prominent bulge, especially in the lower abdomen. This is often less pronounced than swelling or seroma but can still be aesthetically undesirable.
Scar tissue formation is an inherent part of the healing process. While the goal is to minimize visible scarring, some degree of scarring is unavoidable. Hypertrophic scars, which are raised and thickened, or keloid scars, which extend beyond the original wound boundaries, can contribute to a perceived bulge. These are managed with various treatments, including silicone sheeting, steroid injections, or laser therapy.
The position and orientation of the scar itself can also influence the perceived aesthetic outcome. A poorly positioned scar, or one that is excessively wide, can create the illusion of a bulge or asymmetry. Careful surgical planning and meticulous surgical technique are paramount in minimizing these issues.
In some cases, revisional surgery might be considered to address persistent skin redundancy or problematic scarring. This decision is made in consultation with the patient, weighing the potential benefits against the risks and limitations of further surgery. Realistic expectations regarding scar formation and skin laxity are essential for patient satisfaction.
Persistent bulges after a tummy tuck can stem from several factors, ranging from normal post-operative swelling to more complex issues like seromas, diastasis recti, or skin redundancy. Open communication with your surgeon, regular follow-up appointments, and adherence to post-operative instructions are crucial for achieving optimal results and addressing any concerns promptly. Understanding these potential causes allows for appropriate management and realistic expectations regarding the final outcome.
Transform Your Confidence with Surgyteam!
Join the thousands of satisfied patients who have experienced the exceptional care and expertise of Surgyteam’s renowned plastic surgeons. Whether you’re seeking aesthetic enhancements or reconstructive surgery, our dedicated team in Antalya is here to provide you with the highest quality treatment and personalized care.