As a plastic and reconstructive surgeon with extensive experience in aesthetic breast procedures, I understand the profound impact that changes in breast shape and position can have on a woman’s confidence and self-image. One of the most common concerns I address in my practice is breast ptosis, or sagging. It’s a natural consequence of various factors including aging, gravity, pregnancy, breastfeeding, and significant weight fluctuations. For many women, this loss of youthful contour and firmness can be distressing. Fortunately, breast lift surgery, technically known as mastopexy, offers a powerful and effective solution to restore a more youthful, elevated, and aesthetically pleasing breast profile. In this comprehensive guide, I aim to demystify the process of breast lift surgery, offering insights from a surgeon’s perspective and specifically addressing considerations for those contemplating this procedure in Antalya, Turkey.
Table of Contents
Understanding Breast Anatomy and the Aging Process: Why Breasts Change Over Time
To truly appreciate the nuances of breast lift surgery, it is crucial to first understand the intricate architecture of the breast and how it succumbs to the inexorable forces of time and biology. The female breast is a complex structure, primarily composed of glandular tissue (responsible for milk production), fatty tissue, and an intricate network of connective tissues, notably the suspensory ligaments of Cooper (often simply called Cooper’s ligaments). The skin envelope encases these internal components, providing the external shape and support.
The Structural Framework: More Than Just Tissue
The glandular tissue forms the functional core, organized into lobes and lobules that radiate towards the nipple. This tissue is interspersed with fat, the proportion of which varies significantly between individuals and can change throughout a woman’s life. The overall size and softness of the breast are often dictated by the amount of fatty tissue.
The true heroes of breast support, however, are the Cooper’s ligaments. These fibrous bands extend from the deep fascia overlying the pectoralis major muscle (the chest muscle) through the breast tissue, attaching to the dermis (the lower layer of the skin). Think of them as a natural internal scaffolding, helping to hold the breast tissue against gravity.
Blood vessels and nerves also permeate the breast. The vascular supply is robust, primarily from branches of the internal mammary artery and the lateral thoracic artery. The nerve supply is crucial for sensation, particularly to the nipple-areola complex (NAC), the pigmented area surrounding the nipple. Maintaining the integrity of these neurovascular bundles is paramount during surgery to preserve sensation and ensure healthy tissue viability.
Lymphatic drainage, leading to lymph nodes in the axilla (armpit), is also a vital component. Understanding this is important for both surgical planning and post-operative recovery, as disruption can lead to swelling (lymphedema), although this is a rare complication in mastopexy.
The Process of Involution and Ptosis
Over time, several factors contribute to the changes we observe in breast shape and position.
- Aging: As we age, the skin loses its natural elasticity and collagen. The once-tight skin envelope begins to stretch and thin. Simultaneously, the glandular tissue undergoes involution, meaning it shrinks and is often replaced by fat. This shift in tissue composition makes the breast softer and less firm. The combined effect of reduced skin elasticity and decreased structural glandular support leads to sagging.
- Gravity: The constant pull of gravity on breast tissue, especially in larger breasts, gradually stretches the Cooper’s ligaments and the skin envelope over decades.
- Pregnancy and Breastfeeding: Hormonal changes during pregnancy cause the milk glands to enlarge, increasing breast volume. After pregnancy and/or breastfeeding ceases, these glands shrink back down. This rapid expansion and subsequent deflation can significantly stretch the skin and ligaments, contributing to ptosis.
- Weight Fluctuations: Gaining and losing significant amounts of weight can cause the skin to stretch and then become lax when the weight is lost. This is similar to the effect of pregnancy on the breast envelope.
- Genetics: An individual’s genetic predisposition influences skin elasticity and the inherent strength of connective tissues, playing a role in how susceptible they are to developing ptosis.
- Smoking: Smoking impairs blood circulation and damages collagen, accelerating the loss of skin elasticity and hindering healing.
Degrees of Ptosis: Classifying the Sag
As a surgeon, I assess the degree of ptosis to determine the most appropriate surgical technique. We classify ptosis based on the position of the nipple-areola complex (NAC) relative to the inframammary fold (IMF) – the crease beneath the breast – and the lowest point of the breast mound.
Mild Ptosis
In mild ptosis, the nipple is still above the inframammary fold, but it is pointing downwards. The lower pole (the bottom part) of the breast has dropped below the IMF.
Moderate Ptosis
With moderate ptosis, the nipple is at the level of the inframammary fold, but still above the lowest point of the breast mound. The majority of the breast tissue sits below the IMF.
Severe Ptosis
In severe ptosis, the nipple is significantly below the inframammary fold and is often the lowest point of the breast mound. The breast has a markedly elongated and hanging appearance.
Pseudoptosis
This describes a breast where the nipple is still above the inframammary fold, but the lower portion of the breast significantly droops below the IMF. This is often seen in breasts with significant volume, where the sheer weight causes the lower pole to descend, even though the nipple remains relatively high. While not true ptosis by the strict definition of nipple position relative to the IMF, it still presents as a ‘saggy’ appearance that may benefit from a lift.
Understanding the specific degree of ptosis is critical for surgical planning, as it directly influences the required skin removal, tissue reshaping, and ultimately, the resulting scar pattern. My goal is not just to lift the nipple but to reshape the entire breast mound, giving it a more youthful projection and upper pole fullness, while ensuring the nipple is correctly positioned.

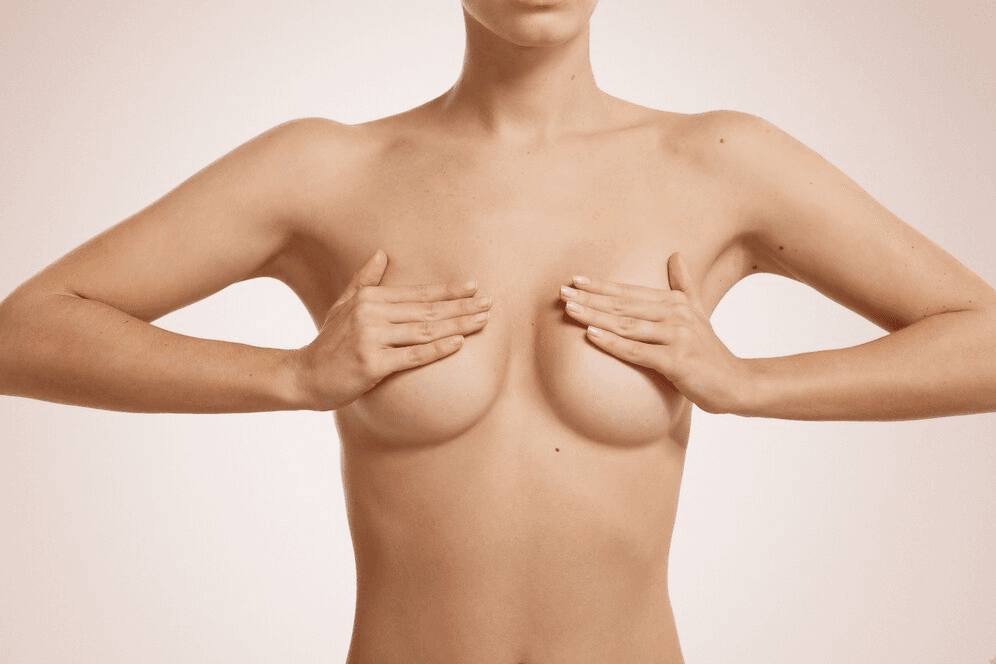
Indications for Mastopexy: Who is a Candidate?
Breast lift surgery is not merely about elevating the nipple; it’s a procedure aimed at reshaping and restoring the aesthetic balance of the breast. As a surgeon, I evaluate potential candidates based on a combination of physical characteristics, medical history, and psychological readiness.
A woman is typically a good candidate for mastopexy if she is bothered by breasts that:
- Have lost their shape and firmness.
- Droop or sag, with nipples pointing downwards.
- Have nipples and areolas that have fallen below the inframammary fold.
- Have stretched areolas.
- Are asymmetrical in terms of shape or position due to sagging.
It’s crucial for candidates to be in good general health and to have realistic expectations about the outcomes. Mastopexy can significantly improve breast contour and position, but it will not change the underlying breast tissue composition or prevent future aging or changes due to pregnancy or weight fluctuations. While scars are an inevitable part of the procedure, a skilled surgeon will place them strategically to be as inconspicuous as possible, and they will fade over time.
Addressing Different Scenarios
Mastopexy is a versatile procedure that can be tailored to various needs:
- Lifting Sagging Breasts Alone: This is the primary indication, focusing solely on raising the nipple, removing excess skin, and reshaping the existing breast tissue.
- Mastopexy with Augmentation: For women who have lost both firmness and volume (common after weight loss or pregnancy), a breast lift can be combined with the insertion of breast implants. This addresses both the sagging and the lack of fullness, particularly in the upper pole. This combined procedure is technically more complex and requires careful planning to ensure proper implant pocket placement and harmonious integration with the lifted tissue.
- Mastopexy with Reduction: Women with large, heavy breasts often experience significant ptosis due to the weight of the tissue. In these cases, a breast reduction (removal of glandular tissue and fat) is performed simultaneously with the lift. This not only elevates the nipple but also reduces the overall size and weight of the breast, alleviating physical symptoms like back and neck pain.
Discussing your specific concerns and goals openly during the consultation is essential. My role is to listen, assess your anatomy, and recommend the surgical approach that is most likely to achieve your desired outcome while prioritizing your safety and long-term well-being.
The Psychological Impact
Beyond the physical changes, breast ptosis can significantly impact a woman’s self-esteem and body image. Many women feel less confident in certain clothing, avoid activities they once enjoyed, or feel self-conscious about their appearance. A successful mastopexy can restore a sense of normalcy and improve self-confidence, allowing women to feel more comfortable and positive about their bodies. It’s important to acknowledge this psychological dimension and ensure that the patient’s motivations for seeking surgery are well-considered and based on a desire for personal improvement, not external pressure.

The Initial Consultation: A Surgeon’s Approach
The initial consultation is perhaps the most critical step in the breast lift journey. It is during this time that I gather essential information, perform a thorough examination, discuss potential surgical approaches, and establish realistic expectations with the patient. This collaborative process is fundamental to a successful outcome.
Gathering Comprehensive Information
My consultation begins with a detailed medical history. I need to know about any existing medical conditions (such as diabetes, heart disease, or autoimmune disorders), previous surgeries (especially any prior breast surgeries or biopsies), allergies, and all medications and supplements the patient is currently taking. Smoking status is particularly important, as smoking significantly increases the risk of complications like delayed wound healing and infection. I also inquire about family history of breast cancer or other breast-related issues. This information helps me assess the patient’s overall health and identify any factors that might increase surgical risk or influence the healing process.
I also delve into the patient’s aesthetic goals. What specifically bothers her about her breasts? What is her desired outcome in terms of shape, position, and firmness? Understanding her motivations and expectations is key to determining if mastopexy is the right procedure for her and to ensuring that her goals are achievable.
The Physical Examination: A Detailed Assessment
The physical examination is a crucial part of the consultation. I examine the breasts in various positions (sitting and standing) to assess:
Breast Size, Shape, and Symmetry
I look at the overall volume, projection, and contour of each breast, noting any existing asymmetries. Minor asymmetry is common in all women, but significant differences need to be evaluated and discussed.
Skin Quality and Elasticity
I assess the skin’s texture, thickness, and elasticity. Skin with good elasticity will contract better after excess skin is removed, leading to a smoother result. Skin that is thin or has significant stretch marks (striae) may not redrape as well, potentially affecting the final contour and requiring modifications to the surgical plan.
Nipple-Areola Complex (NAC) Position
Using anatomical landmarks like the sternal notch (the dip at the base of the neck) and the inframammary fold (IMF), I carefully measure the position of the nipples and areolas. I also assess the size and shape of the areolas, as they can become stretched and enlarged with ptosis. The relationship of the nipple to the IMF and the lowest point of the breast mound helps determine the degree of ptosis, as discussed earlier.
Determining the Degree of Ptosis
Based on the NAC position relative to the IMF and the breast mound, I formally classify the degree of ptosis (mild, moderate, severe, pseudoptosis). This classification is a critical factor in deciding which surgical technique and incision pattern will be most effective in achieving the desired lift and shape.
Palpation
I gently palpate the breast tissue to assess its density and composition (glandular vs. fatty). I also check for any lumps or abnormalities that may require further investigation (e.g., mammography or ultrasound) before surgery can proceed.
Photography and Documentation
Standardized clinical photographs are taken from multiple angles. These photos serve as an objective record of the pre-operative condition, aid in surgical planning, and are used for comparison with post-operative results. These images are confidential and a standard part of the surgical documentation.

Developing a Surgical Plan: Tailoring the Approach
Based on all the information gathered during the history and physical examination, and in collaboration with the patient’s goals, I formulate a personalized surgical plan. This involves:
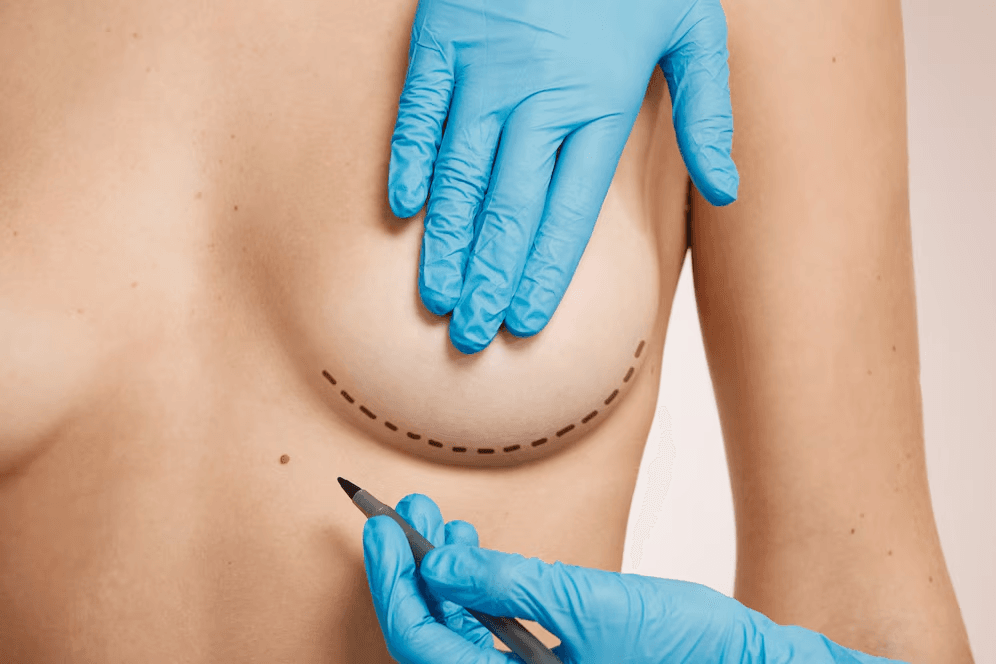
- Choosing the appropriate incision pattern: This is the most visible outcome of the surgery and is chosen based on the degree of ptosis and the amount of skin that needs to be removed.
- Determining the amount of skin to be removed: Precise measurements are taken to ensure adequate lifting without excessive tension on the skin closure.
- Planning the repositioning of the NAC: The new position of the nipple and areola is marked to ensure it is aesthetically pleasing and properly centered on the new breast mound.
- Deciding on tissue reshaping techniques: This may involve glandular plication (folding or stitching the internal breast tissue) to add support and projection, or other techniques to sculpt the breast mound.
- Considering concomitant procedures: If the patient also desires augmentation or reduction, the surgical plan is modified to incorporate these additional steps.
This detailed planning phase is essential to achieving optimal results and minimizing complications. I take the time to explain the proposed plan to the patient, discussing the expected outcomes, the likely scar patterns, and the potential risks and benefits. Informed consent is a process, not just a signature on a form; it involves ensuring the patient fully understands what the surgery entails.
Surgical Techniques in Mastopexy: Crafting the New Contour
The art of breast lift surgery lies in selecting and executing the appropriate surgical technique to achieve the desired elevation and reshape while minimizing visible scarring. There isn’t a single “best” technique; the choice is dictated by the individual patient’s anatomy, the degree of ptosis, the amount of skin elasticity, and the patient’s preference regarding scar placement. All mastopexy techniques involve removing excess skin, repositioning the nipple-areola complex (NAC), and often reshaping the underlying breast tissue.
Incision Patterns: The Scar’s Blueprint
The location and pattern of the surgical incisions determine the resulting scars. I explain the implications of each pattern to the patient, as the visibility of scars is a significant consideration for many.
Peri-Areolar Mastopexy (Donut or Benelli Lift)
This technique involves a circular incision around the border of the areola, with a second, larger concentric circle of incision just outside the first. A ring of skin between these two circles is removed. The skin edges are then brought together like a drawstring purse, tightening the skin around the areola and providing a modest lift.
- Simple Explanation: Think of it like tightening a scrunchie around the nipple. The scar is hidden around the edge of the colored part of the nipple.
- Technical Use: This technique is suitable for patients with minimal ptosis (often pseudoptosis or Grade I ptosis) and good skin elasticity. It offers the advantage of a scar confined to the areola, which is often less noticeable.
- Limitations: The amount of lift achievable with this technique is limited. It is not effective for moderate to severe ptosis or for significantly reshaping the breast mound. It can also sometimes lead to slight flattening of the breast or widening of the areola.
Vertical Mastopexy (Lollipop Lift)
This technique involves a peri-areolar incision combined with a vertical incision extending downwards from the bottom edge of the areola to the inframammary fold (IMF).
- Simple Explanation: This leaves a scar around the nipple area and a straight up-and-down scar from the nipple to the crease under the breast, looking like a lollipop.
- Technical Use: The vertical mastopexy allows for more significant skin removal and reshaping than the peri-areolar lift. It is effective for mild to moderate ptosis. The vertical incision facilitates tightening and lifting of the lower pole of the breast. The vertical scar allows for greater control over breast shape and projection.
- Limitations: It leaves a vertical scar, which is more visible than a peri-areolar scar, although it tends to heal well and fade over time. It may not provide enough lift for severe ptosis.
Inverted T Mastopexy (Anchor Lift)
This is the most powerful technique for lifting and reshaping the breast and is used for moderate to severe ptosis, as well as in most breast reduction procedures. It involves a peri-areolar incision, a vertical incision from the areola to the IMF, and a horizontal incision along the length of the inframammary fold.
- Simple Explanation: This leaves scars around the nipple, a straight line down from the nipple to the crease, and a scar along the crease under the breast, forming an anchor shape.
- Technical Use: The inverted T technique allows for the removal of the largest amount of excess skin from all three dimensions (around the areola, vertically, and horizontally). This enables significant lifting of the NAC, substantial reshaping of the entire breast mound, and reduction of breast width if necessary. It provides the greatest control over the final breast shape and projection.
- Limitations: It results in the most extensive scarring. While the horizontal scar is often hidden by a bra or swimsuit, the peri-areolar and vertical scars are more visible. Scar healing is a key consideration with this technique.
L-shaped and J-shaped Mastopexy
These are variations of the inverted T technique, where the horizontal scar is shorter or curved, forming an L or J shape rather than a full horizontal line. They are used in specific cases to tailor scar placement and potentially reduce the length of the horizontal scar, depending on the amount of skin removal needed.
The Surgical Steps: A Precise Process
Regardless of the incision pattern, the core steps of a mastopexy involve precise tissue manipulation to achieve the desired outcome.
Pre-operative Marking
Before the surgery begins, while the patient is standing and awake, I make detailed markings on the breasts. These markings indicate the planned incision lines, the new position of the NAC, and the areas of skin to be removed. This step is crucial as gravity affects breast position, and marking in a standing position ensures accuracy.
Anesthesia
Mastopexy is typically performed under general anesthesia, ensuring the patient is comfortable and asleep throughout the procedure. A skilled anesthesiologist monitors the patient’s vital signs.
Incisions and Skin Removal
Following the pre-operative markings, incisions are carefully made according to the chosen pattern. The predetermined amount of excess skin is then meticulously removed. The amount and location of skin removal are critical for achieving the desired lift and shape without creating excessive tension on the closure.
Repositioning the Nipple-Areola Complex (NAC)
The NAC, along with its underlying blood supply and nerves, is carefully elevated to its new, higher position on the breast mound. It is vital to maintain the connection to the underlying tissue to preserve blood flow and sensation. This is often done using a “pedicle” – a section of tissue containing the blood vessels and nerves – which is moved along with the NAC.
Reshaping the Breast Mound (Glandular Plication)
After skin removal and NAC repositioning, the remaining breast tissue is often reshaped. This is frequently done through glandular plication, which involves folding or stitching the breast tissue on itself to create a firmer, more projected, and aesthetically pleasing shape. This step provides internal support and contributes significantly to the long-term result. The techniques for plication vary depending on the surgeon’s preference and the specific needs of the breast tissue.
Closing the Incisions
Once the reshaping is complete, the incisions are carefully closed in layers using dissolvable sutures deep within the tissue to provide support and reduce tension, and non-dissolvable or dissolvable sutures on the skin surface. The skin edges are meticulously aligned to promote optimal scar healing. Drains may be placed temporarily to collect any excess fluid, although this is not always necessary depending on the extent of the surgery.
Dressing and Surgical Bra
Sterile dressings are applied, and a supportive surgical bra is placed. This bra helps reduce swelling, provides support to the newly shaped breasts, and is crucial for the initial recovery period.
Choosing the Appropriate Technique: A Tailored Decision
The decision regarding which surgical technique to employ is made during the consultation, based on a thorough assessment of the patient’s anatomy and goals.
- For minimal ptosis and a desire for the least visible scar, the peri-areolar lift might be considered, though its limitations in lift and reshaping must be understood.
- For mild to moderate ptosis requiring more significant lift and shaping, the vertical mastopexy is often the preferred choice, offering a good balance between lift and scar burden.
- For moderate to severe ptosis, where substantial skin removal and reshaping are necessary, the inverted T technique is typically required to achieve a satisfactory outcome, despite the more extensive scarring.
My responsibility as a surgeon is to guide the patient through this decision, explaining the rationale for the recommended technique and ensuring they are comfortable with the expected scar patterns. The goal is always to achieve the best possible aesthetic result with the safest and most appropriate method for that individual.
Combining Mastopexy with Augmentation or Reduction
While the focus of this guide is on mastopexy as a standalone procedure, it’s important to acknowledge that it is frequently combined with other breast surgeries to address multiple concerns simultaneously. Combining procedures adds layers of complexity and requires careful surgical planning to ensure harmonious results and minimize complications.
When Combination is Considered
Combining mastopexy with augmentation or reduction is considered when a patient presents with both sagging and:
- Volume Loss (Augmentation): Women who have experienced significant volume loss due to weight loss, pregnancy, or simply a naturally small breast size, in addition to ptosis, may benefit from adding implants to restore fullness, particularly in the upper pole. The implant provides internal volume that helps to fill the lifted skin envelope.
- Excess Volume (Reduction): Women with large, heavy breasts that are also ptotic often experience physical symptoms related to breast weight. Combining reduction mammaplasty with mastopexy addresses both the size and the sagging, alleviating discomfort and improving overall proportion.
Technical Considerations for Combined Procedures
Performing a combined procedure requires specific surgical expertise:
- Mastopexy with Augmentation: The surgeon must carefully plan the implant pocket (either submuscular, beneath the chest muscle, or subglandular, above the muscle but below the glandular tissue) in relation to the planned breast lift. The size and type of implant must be chosen to complement the amount of lift and reshaping performed. There is a slightly increased risk of complications compared to either procedure alone, such as a higher risk of infection, poor wound healing, or implant malposition if the techniques are not perfectly coordinated. The skin tension created by both lifting and implant placement must be carefully managed.
- Mastopexy with Reduction: The chosen reduction technique must also incorporate the principles of mastopexy to ensure adequate lift and nipple repositioning. The pattern of tissue removal in the reduction must be coordinated with the pattern of skin removal for the lift. This combined procedure is technically demanding as it involves both removing tissue and reshaping the remaining tissue while elevating the NAC.
In both combined scenarios, the surgeon must balance the goals of lifting, reshaping, and adding/removing volume while prioritizing the vascularity of the NAC and ensuring tension-free closure of the incisions. The recovery process for combined procedures can sometimes be slightly longer or involve managing symptoms related to both components of the surgery. During the consultation, if a combined procedure is deemed appropriate, I explain the rationale, the specific techniques involved, and the potential increased risks compared to a standalone mastopexy.
The Surgical Procedure: What to Expect
Undergoing any surgical procedure can be a source of anxiety. Understanding the process from a surgeon’s perspective can help demystify the experience and provide reassurance. Breast lift surgery is typically performed in a hospital or an accredited surgical center, ensuring a safe and sterile environment.
Anesthesia
As mentioned, mastopexy is almost always performed under general anesthesia. This means you will be asleep and feel no pain during the procedure. The anesthesiologist will meet with you before the surgery to review your medical history and discuss the anesthesia plan. They will be present throughout the surgery to monitor your vital signs, including heart rate, blood pressure, oxygen levels, and respiration.
The Operating Room Environment
The operating room is a highly controlled environment. The surgical team, consisting of the surgeon, anesthesiologist, and surgical nurses, works together to ensure your safety and the smooth execution of the procedure. Strict sterile protocols are followed to minimize the risk of infection.
Monitoring During Surgery
Throughout the procedure, your vital signs are continuously monitored. This allows the anesthesiologist to make any necessary adjustments to the anesthesia and ensures that you remain stable. Advanced monitoring equipment is used to track your physiological responses.
Duration of the Procedure
The length of a breast lift surgery varies depending on the complexity of the case and the technique used. A standalone mastopexy typically takes between 2 to 4 hours. If combined with augmentation or reduction, the procedure may take longer. During the consultation, I provide an estimated duration based on the planned surgical approach.
Post-Operative Immediate Care: The Recovery Room
Following the completion of the surgery and the closure of incisions, you will be gently awakened from anesthesia and moved to a recovery room. Here, a dedicated nursing staff will closely monitor you as the effects of anesthesia wear off. They will assess your pain levels, check your vital signs, and watch for any immediate post-operative complications such as excessive bleeding. You may feel groggy, nauseous, or experience some discomfort. Medication will be administered as needed to manage pain and nausea. Once you are stable and fully awake, you will typically be moved to a hospital room or discharged home, depending on the facility’s protocol and the complexity of your surgery. Overnight stay is sometimes recommended, especially for more extensive procedures or if there are any initial concerns.
Potential Risks and Complications
Like any surgical procedure, breast lift surgery carries inherent risks and potential complications. While I take every precaution to minimize these risks, it is crucial for patients to be fully informed about them before making the decision to proceed with surgery. Discussing these possibilities openly during the consultation is a fundamental part of the informed consent process.
General Surgical Risks
These are risks common to most surgical procedures:
Bleeding (Hematoma)
Accumulation of blood under the skin (hematoma) can occur, leading to swelling, bruising, and discomfort. While minor bruising is expected, a significant hematoma may require surgical drainage. Careful surgical technique and post-operative monitoring help minimize this risk.
Infection
Although sterile techniques are strictly followed, there is a small risk of infection at the surgical site. Signs of infection include increased pain, redness, swelling, warmth, and possibly fever. Infections typically require antibiotic treatment and, in some cases, surgical drainage.
Adverse Reaction to Anesthesia
While rare with modern anesthesia, there is a risk of adverse reactions to anesthetic agents. This is why a thorough pre-operative medical evaluation by the anesthesiologist is essential.
Poor Wound Healing
Certain factors, such as smoking, diabetes, poor nutrition, or excessive tension on the incisions, can impair wound healing. Delayed healing can prolong recovery and potentially affect scar appearance.
Scarring
Scars are an unavoidable consequence of any incision. While surgeons strive to place incisions in inconspicuous locations and close them meticulously, individual healing varies. Some individuals may develop hypertrophic scars (thick, raised scars that remain within the boundaries of the original incision) or keloids (scars that grow beyond the original incision boundaries). These are more common in individuals with darker skin tones. Scar management techniques can help improve their appearance over time.
Specific Mastopexy Risks
These risks are more directly related to the nature of breast lift surgery:
Changes in Nipple or Breast Sensation
Changes in sensation in the nipples, areolas, or breast skin are common after mastopexy. This can manifest as decreased sensation, increased sensitivity, or numbness. In most cases, sensation gradually returns over several months, but permanent changes in sensation, including complete loss of sensation or chronic pain, are possible, though less common. The risk is influenced by the surgical technique used and the manipulation of the nerve supply to the NAC.
Asymmetry
While surgeons aim for symmetry, perfect symmetry is rarely achieved in nature or surgery. Minor degrees of asymmetry in breast size, shape, or nipple position can occur after mastopexy. Significant asymmetry that is aesthetically displeasing may require revision surgery. Pre-existing asymmetry may also persist or become more noticeable after surgery.
Scarring (Detailed)
As mentioned, scars are inherent.
Keloids and Hypertrophic Scars
- Simple Explanation: These are scars that become lumpy and raised, sometimes spreading beyond the cut lines.
- Technical Explanation: Hypertrophic scars are raised and thickened but stay within the confines of the original incision. Keloids are more aggressive and extend beyond the boundaries of the wound. Both are due to an overproduction of collagen during the healing process. They can be itchy, painful, and aesthetically undesirable. Management may include silicone sheets or gels, corticosteroid injections, or revision surgery.
Delayed Wound Healing or Wound Dehiscence
In some cases, the surgical incisions may be slow to heal, or a portion of the wound may open up (dehiscence). This requires diligent wound care and can prolong the recovery period. Factors like smoking, infection, or excessive tension on the wound edges increase this risk.
Fat Necrosis
This occurs when fatty tissue within the breast dies due to insufficient blood supply, forming firm lumps. Fat necrosis can sometimes be mistaken for a suspicious lesion and may require further investigation or even surgical removal.
Seroma
Accumulation of clear fluid (seroma) under the skin can occur. Small seromas may resolve on their own, while larger ones may require drainage with a needle and syringe.
Unsatisfactory Aesthetic Result
Despite careful planning and execution, the final aesthetic outcome may not fully meet the patient’s expectations or the surgeon’s goals. This could relate to the shape, size, projection, or position of the breasts or nipples. Realistic expectations are crucial to avoid dissatisfaction.
Need for Revision Surgery
In some instances, a secondary procedure (revision surgery) may be necessary to address complications, correct asymmetry, or improve the aesthetic outcome. This is not uncommon in plastic surgery and should be discussed as a possibility, though it is not the goal.
Minimizing Risks: A Collaborative Effort
Minimizing these risks is a collaborative effort between the surgeon and the patient.
- Surgeon’s Role: Careful patient selection, thorough pre-operative planning, meticulous surgical technique, and appropriate post-operative care instructions are key responsibilities of the surgeon.
- Patient’s Role: The patient plays a vital role by providing a complete and accurate medical history, following pre-operative instructions (such as quitting smoking well in advance of surgery), adhering strictly to post-operative care instructions, and attending all follow-up appointments.
A comprehensive discussion of risks during the consultation allows the patient to make an informed decision about whether to proceed with breast lift surgery.
Recovery and Post-Operative Care
The recovery period following breast lift surgery requires patience, adherence to instructions, and careful attention to your body’s signals. As your surgeon, I provide detailed post-operative instructions designed to optimize healing, minimize complications, and ensure the best possible outcome.
Immediate Post-Op: Managing Discomfort and Support
Upon waking in the recovery room, you will likely experience some discomfort, swelling, and bruising. Pain medication will be administered to manage this.
Pain Management
Prescription pain medication will be provided to control discomfort. It’s important to take this medication as directed. Over-the-counter pain relievers may also be recommended for milder discomfort as your recovery progresses.
Drains (If Used)
If drains were placed during surgery to collect excess fluid, you will be instructed on how to care for them and measure the output. Drains are typically removed within a few days when the fluid output significantly decreases.
Surgical Bra
You will be fitted with a supportive surgical bra immediately after the procedure. This bra provides essential compression and support to the healing tissues, helps reduce swelling, and stabilizes the breasts in their new position. You will typically need to wear this bra continuously for several weeks, as instructed.
First Few Days/Weeks: Managing Symptoms and Rest
The first few days after surgery are crucial for initial healing.
Swelling and Bruising
Significant swelling and bruising are expected. This can extend to the chest wall and even the upper abdomen. Cold compresses can help reduce swelling in the initial 24-48 hours. Swelling gradually subsides over several weeks to months.
Discomfort
You will experience a feeling of tightness, soreness, and discomfort in the chest area. This is normal and managed with pain medication.
Restricted Activity
During the initial recovery period, you will need to significantly restrict your activity. This includes avoiding lifting, pushing, or pulling with your arms and upper body. Strenuous activities and exercise are strictly prohibited. You will need assistance with daily tasks.
Activity Restrictions: Gradual Return
A gradual return to normal activities is essential to prevent complications and ensure proper healing.
Lifting and Strenuous Exercise
Avoid lifting anything heavier than a few pounds for at least 4-6 weeks. Strenuous exercise, including running, jumping, and heavy weightlifting, should be avoided for a similar period, or longer, as advised. Returning to activities too soon can cause pain, swelling, and potentially disrupt the healing incisions.
Driving
You should not drive while taking prescription pain medication or until you are comfortable and able to react quickly and safely. This is typically not for at least a week or two.
Wound Care and Dressing Changes
You will receive specific instructions on how to care for your incisions. This may involve keeping them clean and dry, changing dressings, and applying antibiotic ointment. Follow these instructions meticulously to promote healing and prevent infection.
Follow-Up Appointments
Scheduled follow-up appointments with me are vital. During these visits, I will monitor your healing progress, remove sutures (if non-dissolvable ones were used), check for any signs of complications, and provide further guidance on your recovery. Do not miss these appointments.
Returning to Work and Normal Activities: A Variable Timeline
The timeline for returning to work and normal activities varies depending on the individual’s healing rate, the extent of the surgery, and the nature of their job.
- Many patients with sedentary jobs can return to work within 1-2 weeks, provided they avoid strenuous activity.
- Jobs requiring physical labor or heavy lifting will require a longer recovery period, potentially 4-6 weeks or more.
Listen to your body and do not push yourself too hard, even if you feel like you are recovering quickly.
Scar Management: Promoting Fading
Once the incisions have healed and the sutures are removed, scar management can begin to help the scars mature and fade.
Silicone Sheets or Gels
Applying silicone sheets or gels to the scars is often recommended. These products can help flatten, soften, and reduce the redness of scars over time.
Massage
Gentle massage of the scars, once they are fully healed, can also help to soften them and improve their appearance.
Sun Protection
Protecting scars from sun exposure is crucial for at least a year, as UV radiation can cause hyperpigmentation (darkening) of the scars. Use sunscreen with a high SPF or keep the scars covered.
Scar maturation is a lengthy process, often taking 12 to 18 months for the scars to reach their final appearance. Be patient and consistent with scar management techniques.
Emotional Recovery: Adjusting to Your New Body
Physical recovery is only one aspect; emotional recovery is also important. It takes time to adjust to changes in body image. It’s normal to experience a range of emotions, from excitement about the results to frustration with the limitations of recovery. Having realistic expectations from the outset and understanding that the final results take time to become apparent can help manage this. If you experience significant mood changes or concerns, discuss them with me or seek support from a mental health professional.
Long-Term Results and Expectations
The immediate post-operative appearance of your breasts will not be the final result. Significant swelling and bruising will distort the shape, and the tissues will need time to settle. Understanding the long-term trajectory of healing and the factors that can influence the longevity of your results is important.
The Maturation Process: Time Reveals the Outcome
It typically takes several months, often 6 to 12 months, for the majority of swelling to subside and for the breast tissues to soften and settle into their final shape. During this time, the shape and contour of your breasts will continue to refine.
Scars also undergo a maturation process. Initially, they may be red, raised, and firm. Over the course of 1 to 2 years, they should gradually flatten, soften, and fade to a less conspicuous color, often becoming pale and subtle. Individual healing characteristics play a significant role in scar appearance.
Longevity of Results: Not Immune to Future Changes
Breast lift surgery provides a significant and long-lasting improvement in breast shape and position, but it does not halt the aging process or make your breasts immune to future changes. Factors that contributed to the initial ptosis can still have an effect over time:
- Aging and Gravity: The natural effects of aging and gravity will continue to act on the breast tissue and skin, potentially leading to some degree of recurrent sagging over many years or decades.
- Weight Changes: Significant weight gain and subsequent loss can stretch the skin and tissues, impacting the longevity of the lift. Maintaining a stable weight is beneficial for preserving your results.
- Pregnancy and Breastfeeding: Future pregnancies and breastfeeding can again cause changes in breast volume and skin elasticity, potentially affecting the outcome of a previous mastopexy. Many surgeons advise completing childbearing before undergoing a breast lift for the longest-lasting results, although this is a personal decision.
Maintaining Your Results: Supportive Measures
While you cannot completely prevent future changes, certain measures can help support and potentially extend the longevity of your mastopexy results:
Healthy Weight
Maintaining a stable, healthy weight avoids the stretching and laxity that can result from significant weight fluctuations.
Supportive Bras
Wearing supportive bras, especially during physical activity, can help counteract the effects of gravity and provide external support to the breast tissues and skin.
Healthy Lifestyle
Overall good health, including a balanced diet and avoiding smoking, supports skin elasticity and tissue health, which can contribute to maintaining your results.
It is important to have realistic long-term expectations. While mastopexy can turn back the clock on breast aging and sagging, it does not stop time. Most patients are very satisfied with the improvement in their breast contour and the restoration of a more youthful appearance for many years following the surgery.
Choosing Antalya for Your Breast Lift Surgery
Antalya, a vibrant city on Turkey’s Mediterranean coast, has emerged as a significant destination for medical tourism, particularly for plastic surgery procedures like breast lifts. Several factors contribute to its appeal, offering patients a combination of high-quality medical care, experienced surgeons, competitive costs, and an attractive environment for recovery.
The Appeal of Antalya for Medical Tourism
Antalya’s growing popularity as a medical tourism hub is driven by:
- Quality Clinics and Hospitals: Many hospitals and clinics in Antalya are modern, well-equipped facilities that adhere to international standards of safety and care. Some hold international accreditations, such as Joint Commission International (JCI), which signifies a commitment to rigorous quality and patient safety standards.
- Experienced Surgeons: Turkey has a strong tradition of plastic surgery, and many surgeons practicing in Antalya are highly qualified, often trained internationally, and possess extensive experience in aesthetic procedures, including mastopexy. They are often members of national and international plastic surgery societies.
- Cost-Effectiveness: Compared to Western Europe, North America, and other developed countries, the cost of plastic surgery in Antalya is often significantly lower. This is due to various factors, including lower overhead costs, favorable exchange rates, and a competitive market. However, lower cost does not necessarily equate to lower quality; it reflects economic differences.
- Recovery Environment: Antalya offers a pleasant climate and a relaxing environment, which can be conducive to a comfortable recovery. Patients can recuperate in a tranquil setting, away from the stresses of their daily lives. Many clinics offer packages that include accommodation in comfortable hotels, facilitating the recovery process.
What to Look for in a Clinic/Surgeon in Antalya
If you are considering breast lift surgery in Antalya, thorough research and careful selection of your surgeon and clinic are paramount. Here are key factors to evaluate:
Board Certification/Qualifications
Ensure that the surgeon is a qualified plastic and reconstructive surgeon. Look for evidence of board certification or membership in relevant national or international plastic surgery associations. This indicates they have met specific training and ethical standards.
Experience Specifically in Mastopexy
While a surgeon may be board-certified, inquire about their specific experience with breast lift procedures. How many mastopexy surgeries have they performed? Do they specialize in aesthetic breast surgery? Reviewing their before-and-after photo gallery can provide insights into their results for cases similar to yours.
Accreditation of the Facility
Verify that the hospital or clinic where the surgery will be performed is accredited. International accreditations like JCI are a strong indicator of high standards of patient care and safety. Local accreditations are also important.
Patient Testimonials and Before-and-After Photos
Seek out patient testimonials or reviews to gauge the experiences of others. Reviewing the surgeon’s before-and-after photo gallery is crucial to assess the quality of their work and see results from patients with similar pre-operative conditions. Remember that every individual’s results will vary.
Consultation Process
A good clinic and surgeon will offer a thorough and informative consultation process. Communication should be clear and transparent. The surgeon should listen to your goals, perform a detailed examination, explain the proposed surgical plan, discuss the risks and benefits, and answer all your questions patiently. Effective communication is vital, especially when traveling for surgery. Many clinics catering to international patients have translators or patient coordinators who can assist with communication.
Package Details
Many medical tourism providers in Antalya offer packages that include the surgical fee, hospital stay, anesthesia fees, and sometimes accommodation and airport transfers. Clearly understand what is included and what is not in the quoted price to avoid hidden costs.
Logistical Considerations for Traveling for Surgery
Undergoing surgery abroad requires additional logistical planning:
Travel and Accommodation
Book your flights and accommodation well in advance. Ensure the accommodation is comfortable and suitable for post-operative recovery (e.g., easy access, comfortable bed).
Duration of Stay Needed for Recovery
You will need to stay in Antalya for a sufficient period to allow for initial healing and follow-up appointments. This typically ranges from 7 to 14 days, depending on the extent of the surgery and your individual healing. Plan your return travel only after getting clearance from your surgeon.
Language Barrier
While many clinics cater to international patients and have English-speaking staff or translators, be prepared for potential language differences in other interactions outside the clinic. Having a translation app on your phone can be helpful.
Choosing Antalya can be an excellent option for breast lift surgery, offering access to skilled surgeons and quality facilities at a more accessible price point. However, the due diligence in researching and selecting your medical provider remains essential.
Understanding Costs in Antalya
The cost of breast lift surgery is a significant factor for many patients considering medical tourism. While Antalya offers competitive pricing compared to many Western countries, the exact cost can vary considerably depending on several factors. It’s crucial to get a detailed and transparent quote from the clinic or surgeon.
Factors Influencing Cost
The total cost of a breast lift in Antalya is influenced by:
Technique Used
More complex techniques, such as the inverted T mastopexy, which require more extensive dissection and reshaping, may cost more than a simpler peri-areolar lift.
Complexity of the Case
If your case is more complex due to significant ptosis, asymmetry requiring detailed correction, or if it’s a revision surgery, the cost may be higher due to the increased surgical time and effort required.
Surgeon’s Experience and Reputation
Highly experienced and reputable surgeons often command higher fees, which reflects their expertise and track record of successful outcomes.
Clinic/Hospital Fees
The cost includes fees for the surgical facility (operating room, equipment), anesthesia, and potentially an overnight hospital stay if required. The type and accreditation of the facility can influence the cost.
Inclusion of Other Services
Medical tourism packages often bundle various services. The cost will vary depending on whether accommodation, airport transfers, pre-operative tests, post-operative garments, and follow-up visits are included in the price.
Why it Might Be More Cost-Effective
The lower cost of breast lift surgery in Antalya compared to many other countries is primarily due to:
- Lower Operating Costs: The general cost of doing business, including facility overheads, staff salaries, and medical supplies, can be lower in Turkey.
- Favorable Exchange Rates: The exchange rate between your home currency and the Turkish Lira can make medical services more affordable.
- Competitive Market: The growing medical tourism sector in Antalya has created a competitive market among clinics and hospitals, which can help keep prices competitive.
It’s important to reiterate that a lower cost does not automatically mean lower quality. Many clinics and surgeons in Antalya maintain very high standards. The cost savings are often a reflection of economic differences rather than a compromise on quality or safety.
Importance of Getting a Detailed Quote
Always request a detailed, itemized quote from the clinic. This should clearly outline all the costs included in the price (surgeon’s fee, anesthesia fee, hospital fee, etc.) and specify any potential additional costs (e.g., cost of post-operative medication, follow-up consultations after returning home, costs associated with potential complications). Understanding the full financial picture is essential for planning your medical trip.
Legal and Ethical Considerations
Undergoing surgery, especially in a foreign country, involves important legal and ethical considerations. As your surgeon, I adhere to strict ethical guidelines and legal requirements to ensure your safety, rights, and informed decision-making.
Informed Consent Process
The foundation of ethical medical practice is informed consent. This is a continuous process that begins during the initial consultation and continues until you are ready to proceed with surgery.
Explaining the Procedure
I will explain the proposed breast lift procedure in detail, including the planned surgical technique, the expected outcomes, and the likely scar patterns.
Discussing Risks, Benefits, and Alternatives
I will have an open and honest discussion about the potential risks and complications of the surgery, as well as the anticipated benefits. I will also discuss alternative treatment options, including non-surgical approaches (though for significant ptosis, surgical intervention is typically the only effective method) and the option of not having surgery at all.
Ensuring Understanding
It is my responsibility to ensure that you fully understand all aspects of the procedure, including the potential outcomes and risks. I encourage you to ask questions and voice any concerns you may have. You should feel comfortable that all your questions have been answered satisfactorily before you make a decision.
Voluntary Decision
The decision to undergo surgery must be entirely voluntary and free from coercion. You have the right to take your time, seek second opinions, and ultimately decide against the surgery at any point.
Signing a consent form is a formal documentation of this process, confirming that the discussion took place and you understand and agree to the proposed treatment. However, the ethical responsibility goes beyond the signature; it’s about ensuring genuine understanding and autonomy.
Patient Rights
As a patient undergoing medical treatment in Turkey, you have certain rights. These typically include:
- The right to receive clear and understandable information about your medical condition and treatment options.
- The right to make decisions about your own healthcare.
- The right to privacy and confidentiality of your medical information.
- The right to a second opinion.
- The right to safe and quality medical care.
Familiarize yourself with patient rights in Turkey, which are generally aligned with international standards. Reputable clinics and hospitals will operate in a manner that respects these rights.
Medical Malpractice Considerations
While the vast majority of surgical procedures are performed safely and successfully, medical errors can occur. If you believe you have been a victim of medical malpractice, seeking legal advice is an option. Understanding the legal framework for medical malpractice claims in Turkey can be complex, particularly for international patients. This is another reason why choosing a reputable and accredited facility with experienced surgeons is crucial, as it significantly reduces the likelihood of such issues.
Detailed Anatomy Revisited: A Deeper Dive
To further appreciate the complexity of breast lift surgery and the surgeon’s considerations, let’s revisit breast anatomy with a more technical lens, focusing on structures particularly relevant to mastopexy outcomes.
Cooper’s Ligaments: More Than Just Bands
While previously described as simple suspensory ligaments, Cooper’s ligaments (ligamenta suspensoria mammaria) are a much more intricate network. They are fibrous septa that extend from the clavipectoral fascia (a layer of connective tissue associated with the chest muscles and clavicle) through the breast parenchyma (glandular and fatty tissue) to the deep layer of the dermis (skin). Their function is to support the breast tissue and maintain the connection between the skin envelope and the underlying chest wall. As mentioned, these ligaments stretch and weaken with age, gravity, and other factors, contributing significantly to ptosis. During mastopexy, surgeons aim to reposition and sometimes reinforce these internal structures to provide better long-term support for the lifted breast.
Blood Supply: Nourishing the Tissues
Maintaining adequate blood supply to the breast tissue and the repositioned nipple-areola complex (NAC) is critical for healing and tissue viability. The primary arterial supply to the breast is from:
- Internal Mammary Artery: Branches of this artery, which runs beneath the sternum (breastbone), supply the medial (inner) part of the breast.
- Lateral Thoracic Artery: Branches of this artery, which runs along the side of the chest, supply the lateral (outer) part of the breast.
- Intercostal Arteries: Branches from the arteries between the ribs also contribute to the blood supply.
During mastopexy, particularly when elevating the NAC on a pedicle, the surgeon must carefully preserve the arterial supply to this critical structure. The specific design of the pedicle (the strip of tissue carrying the NAC) is based on ensuring sufficient blood flow from these source vessels. Compromised blood supply can lead to complications such as nipple necrosis (tissue death).
Venous drainage largely parallels the arterial supply, with veins draining into the internal mammary and axillary veins. Efficient venous drainage is necessary to prevent post-operative swelling and congestion.
Nerve Innervation: Preserving Sensation
Sensation in the breast and NAC is provided by branches of the intercostal nerves (nerves between the ribs) and the supraclavicular nerves (nerves from the neck/shoulder area). The sensation of the NAC is primarily supplied by branches of the 4th, 5th, and 6th intercostal nerves. These nerves travel through the breast tissue.
During mastopexy, especially with significant tissue rearrangement and NAC repositioning, there is a risk of injuring these delicate nerves, leading to changes in sensation. The surgeon takes great care to preserve these nerve bundles within the pedicle when elevating the NAC. While temporary changes in sensation are common due to swelling and nerve stretching, permanent numbness or altered sensation is a recognized risk.
Lymphatic Drainage: Clearing Fluids
Lymphatic vessels in the breast drain fluid and waste products, primarily to the axillary lymph nodes (located in the armpit). There is also drainage to internal mammary lymph nodes. Understanding the lymphatic pathways is important, though significant disruption leading to chronic lymphedema is rare in mastopexy alone. Temporary post-operative swelling is more related to surgical trauma and fluid accumulation.
Pectoralis Muscle Relationship
The breast lies directly over the pectoralis major muscle. While the breast tissue is separate from the muscle fascia, the position and contour of the pectoralis muscle can influence the overall shape of the chest wall and indirectly affect the appearance of the breast, particularly after augmentation or when assessing the foundation for the breast mound. During mastopexy, the surgeon is primarily working with the breast tissue and skin, but an awareness of the underlying muscle is part of the anatomical understanding.
A detailed understanding of these anatomical structures and their function is fundamental for a plastic surgeon performing mastopexy. It guides surgical planning, technique selection, and efforts to preserve function (like sensation) and promote optimal healing.
Specific Technical Nuances of Mastopexy: Refining the Craft
Moving beyond the basic incision patterns, the actual execution of a mastopexy involves numerous technical nuances that distinguish a skilled surgeon and contribute to the final aesthetic outcome. These details involve precise tissue handling, meticulous suturing, and a deep understanding of how tissues will heal and settle.
Skin Resection Patterns in More Detail
The amount and shape of skin removed are precisely planned based on the pre-operative markings and the degree of ptosis.
- Peri-Areolar: A ring of skin is removed around the areola. The width of this ring determines the amount of skin tightening around the areola.
- Vertical: In addition to the peri-areolar skin removal, a fusiform (spindle-shaped) section of skin is removed below the areola, extending vertically to the IMF. The width and length of this vertical segment determine the amount of vertical skin tightening and the resulting scar.
- Inverted T: This involves removing a fusiform vertical segment and a crescent or elliptical segment of skin along the IMF. The shape and size of these segments are meticulously planned to achieve the desired lift and contour. The excess skin in the lateral (outer) and medial (inner) aspects of the lower breast is also removed.
Precise measurement and careful excision of the skin are critical. Removing too little skin will result in an inadequate lift, while removing too much can lead to excessive tension on the closure, potentially causing delayed healing, wider scars, or even tissue necrosis.
Glandular Plication Techniques: Internal Sculpting
Reshaping the underlying breast tissue is often as important as skin removal for creating a long-lasting, aesthetically pleasing result. Glandular plication involves using sutures to gather, fold, or reshape the glandular and fatty tissue of the breast.
- Central Mound Plication: Sutures can be placed to gather the tissue towards the center of the breast, creating a more projected and conical shape.
- Lateral and Medial Plication: Tissue on the sides can be plicated to narrow the base of the breast and improve projection.
- Superior Plication: Tissue in the lower pole can be folded upwards and secured to the chest wall or upper breast tissue to provide internal support and fill the upper pole.
These internal sutures provide structural support to the lifted breast mound, helping to resist the effects of gravity over time and contributing to a more stable and durable result. The specific plication techniques used will depend on the patient’s breast anatomy, the amount of tissue, and the desired final shape.
NAC Transposition: Preserving Vitality
Elevating the nipple-areola complex (NAC) to its new position requires preserving its blood supply and nerve innervation. This is achieved by raising the NAC on a “pedicle,” a strip of underlying breast tissue that contains the necessary blood vessels and nerves.
- Superior Pedicle: The NAC is elevated on a pedicle based superiorly (towards the chest wall/clavicle). This is a common technique, particularly in mastopexy with augmentation, as it preserves the blood supply from the superior vessels.
- Inferior Pedicle: The NAC is elevated on a pedicle based inferiorly (towards the IMF). This is often used in breast reduction techniques combined with mastopexy.
- Central Pedicle: The NAC is elevated on a cylindrical pedicle of tissue from the central breast.
- Dermal Pedicle: The NAC is elevated on a pedicle primarily composed of dermis and some subcutaneous tissue, relying on the subdermal vascular plexus.
The choice of pedicle depends on the amount of lift required, the amount of tissue to be removed or rearranged, and the surgeon’s preference and experience. Meticulous dissection to preserve the pedicle and avoid tension on the vascular and nerve supply is paramount.
Managing Different Breast Tissue Types
The composition of the breast tissue (dense and glandular versus soft and fatty) influences surgical planning.
- Dense/Glandular Breasts: These breasts tend to hold their shape better but may be more challenging to reshape with plication alone.
- Fatty/Soft Breasts: These breasts are more prone to sagging but may be easier to reshape internally. Significant fat removal may be necessary in some areas to achieve the desired contour.
The surgeon must adapt their techniques to the specific tissue characteristics to achieve optimal results.
Addressing Asymmetry During Surgery
Existing breast asymmetry is common. During mastopexy, the surgeon can often improve symmetry by:
- Removing slightly different amounts of skin from each breast.
- Using different plication techniques on each side.
- Adjusting the position of the NAC on each breast.
- In cases of significant volume asymmetry, combining mastopexy on one side with mastopexy and augmentation/reduction on the other.
Achieving perfect symmetry is challenging, and minor differences may persist, but significant improvements are often possible.
These technical details highlight the complexity and artistry involved in breast lift surgery. It is a procedure that requires not only anatomical knowledge but also surgical skill, judgment, and an aesthetic eye to sculpt the breasts into a harmonious and youthful contour.
Advanced Mastopexy Considerations
Beyond the standard techniques, there are certain complex scenarios and additional procedures that may be addressed during or in conjunction with mastopexy.
Dealing with Tubular Breasts
Tubular breasts (also known as constricted breasts or tuberous breast deformity) are a congenital condition characterized by a constricted breast base, herniation of breast tissue into the areola, and often significant ptosis even at a young age. Correcting tubular breasts often requires specific techniques beyond a standard mastopexy, including:
- Releasing the constricting fibrous band at the breast base.
- Redistributing or scoring the breast parenchyma (tissue) to allow it to expand into a more rounded shape.
- Addressing the enlarged and often herniated areola.
- Often, augmentation with implants is required to provide sufficient volume and fill the expanded skin envelope after the constriction is released.
Mastopexy techniques, usually the vertical or inverted T, are then used to lift and reshape the breast once the underlying deformity has been corrected. This is a complex type of mastopexy that requires specialized experience.
Revision Mastopexy
Revision surgery is performed to address issues arising from a previous breast lift, such as recurrent ptosis, asymmetry, undesirable scarring, or dissatisfaction with the shape or position. Revision mastopexy can be more challenging than the initial procedure due to altered anatomy, scar tissue, and potentially compromised blood supply. The surgeon must carefully evaluate the previous surgery and tailor the revision technique accordingly. It may involve further skin removal, adjustments to the internal plication, or repositioning of the NAC.
Nipple Reduction or Areola Reduction/Reshaping
With ptosis, the areolas often become stretched and enlarged. During mastopexy, the areola size can be reduced by removing a ring of skin from the outer edge of the areola. The desired size is typically marked pre-operatively.
Nipple reduction can also be performed simultaneously if the nipples are considered too long or wide. This involves surgically reducing the size of the nipple while preserving sensation and the ability to breastfeed if applicable (although the primary goal of mastopexy is aesthetic, and preservation of breastfeeding is not guaranteed).
These additional procedures allow for a more comprehensive aesthetic improvement, addressing not only the position and shape of the breast but also the aesthetics of the nipple-areola complex.
Recovery Phases in Detail
Breaking down the recovery period into phases can help patients understand the progression of healing and what to expect at different points in time. While individual recovery varies, this general timeline provides a useful framework.
Week 1: Initial Healing and Acute Symptoms
The first week is the most challenging phase of recovery.
- Pain and Discomfort: Pain is typically managed with prescription medication. Discomfort is characterized by tightness, soreness, and possibly burning sensations.
- Swelling and Bruising: Swelling and bruising are most pronounced during this week.
- Limited Mobility: Movement of the arms and upper body is restricted. You will need assistance with tasks like showering, dressing, and preparing meals.
- Fatigue: It is common to feel tired as your body dedicates energy to healing.
- Drains (If Present): If drains were inserted, they are usually removed within the first few days.
- Wound Care: Dressings will need to be changed as instructed. Incisions may be covered with sterile tape or bandages.
During this week, focus on rest, pain management, and following all post-operative instructions meticulously. Avoid showering until cleared by your surgeon, and keep incisions dry.
Weeks 2-4: Gradual Improvement and Increased Activity
During this period, you will start to feel significantly better, although swelling and bruising will still be present to some degree.
- Decreased Pain: Pain levels should decrease, and you may be able to transition to over-the-counter pain relievers.
- Reduced Swelling and Bruising: Swelling and bruising will gradually subside.
- Increased Mobility (with Caution): You can gradually increase your activity level, but still avoid strenuous activities and heavy lifting. Light walking is encouraged to promote circulation.
- Return to Sedentary Work: If your job is sedentary, you may be cleared to return to work during this period.
- Scar Care Begins: Once incisions are fully closed and cleared by your surgeon, you can begin scar management techniques like applying silicone sheets or gels.
Continue wearing your surgical bra as instructed. Avoid raising your arms completely overhead.
Months 1-3: Continued Healing and Resumption of Most Activities
By the end of the first month, most of the significant swelling should have resolved, and you will start to see the initial shape of your lifted breasts.
- Swelling Continues to Decrease: Residual swelling will gradually diminish.
- Scars Begin to Mature: Scars will still be visible but may start to soften and flatten.
- Resumption of Most Activities: You can gradually return to most normal activities, including light to moderate exercise, as cleared by your surgeon. Avoid activities that cause pain or discomfort in the chest area.
- Wearing Regular Bras (with Support): You may be allowed to transition to supportive non-underwire bras. Avoid underwire bras for several months as they can irritate healing incisions.
Continue with scar management. Listen to your body and don’t rush your return to full activity.
Months 3-12: Scar Maturation and Final Results Emerge
Over the next several months, your breasts will continue to settle, and the final results will become more apparent.
- Final Shape and Position: The breasts will soften, and the shape and position will stabilize.
- Scar Maturation: Scars will continue to fade and become less noticeable.
- Resumption of All Activities: By this point, you should be able to resume all your usual activities, including strenuous exercise.
Continue protecting your scars from the sun.
Beyond 1 Year: Long-Term Outcome and Maintenance
By one year post-surgery, your scars should be largely mature, and your results should be stable.
- Stable Results: Your breast shape and position should remain consistent, subject to the effects of aging and other factors over time.
- Mature Scars: Scars will have reached their final appearance.
Continue to maintain a healthy lifestyle and wear supportive bras to help preserve your results over the long term. Remember that while the lift is long-lasting, the natural aging process will continue.
Patient Selection Criteria: Ensuring Suitability
As a surgeon, carefully selecting patients for breast lift surgery is paramount to ensuring safety, achieving satisfactory outcomes, and minimizing the risk of complications or dissatisfaction. Not everyone who desires a breast lift is an ideal candidate. Beyond the physical indications of ptosis, several factors are considered to determine a patient’s suitability.
Medical Contraindications
Certain medical conditions can increase the risks associated with surgery and anesthesia, making mastopexy potentially unsafe. These are considered contraindications:
- Significant Uncontrolled Medical Conditions: Patients with poorly controlled diabetes, severe heart disease, lung disease, or autoimmune disorders may be at higher risk of complications during and after surgery.
- Active Infections: Any active infection in the body needs to be treated and resolved before elective surgery is performed.
- Bleeding Disorders: Conditions that affect blood clotting can increase the risk of excessive bleeding and hematoma.
- Certain Medications: Some medications, such as blood thinners, may need to be stopped or adjusted before surgery.
- Active Smoking: As repeatedly emphasized, smoking significantly impairs healing and increases complication risks (infection, delayed healing, skin necrosis). Patients are strongly advised to quit smoking several weeks before and after surgery.
A thorough medical history and physical examination, potentially including pre-operative tests (blood work, EKG), are conducted to identify any potential medical contraindications.
Psychological Readiness and Realistic Expectations
The patient’s psychological state and their expectations about the surgical outcome are equally important.
- Realistic Expectations: Patients must have a clear understanding of what mastopexy can and cannot achieve. It can lift and reshape, but it will not drastically change breast size (unless combined with augmentation or reduction), create perfect symmetry, or stop the effects of aging. Unrealistic expectations are a common cause of patient dissatisfaction.
- Emotional Stability: Patients should be emotionally stable and not undergoing significant stress or life changes. Surgery should not be sought to solve underlying psychological issues or relationship problems.
- Motivation for Surgery: The motivation for surgery should be personal desire for self-improvement rather than pressure from others.
- Understanding of Scars: Patients must be prepared for and accepting of the unavoidable scarring that results from mastopexy.
During the consultation, I assess the patient’s psychological readiness and work to ensure their expectations are realistic. If I have concerns about a patient’s psychological state or expectations, I may recommend counseling or further discussion before proceeding with surgery.
Importance of Being a Non-Smoker
This point warrants reiteration due to its critical impact on surgical outcomes. Smoking constricts blood vessels, reducing blood flow to the tissues. This severely impairs the body’s ability to heal and increases the risk of:
- Delayed wound healing
- Wound dehiscence (opening)
- Infection
- Skin necrosis (tissue death), particularly of the nipples and surrounding skin, which rely on adequate blood supply from a pedicle.
Patients who smoke must quit at least 4-6 weeks before surgery and remain smoke-free throughout the critical healing period. Nicotine replacement products should also be avoided as they can still have vasoconstrictive effects. I will not perform elective breast surgery on active smokers due to the significantly elevated risks.
Weight Stability
Significant weight fluctuations before or after surgery can negatively impact the results. Patients should be at a stable, healthy weight before considering mastopexy. Planning surgery during a period of significant weight loss or gain is generally not advised, as the final results can be compromised. Maintaining a stable weight after surgery is also important for preserving the long-term outcome.
By carefully evaluating these patient selection criteria, I can identify individuals who are most likely to undergo surgery safely, heal well, and be satisfied with their results. Patient safety and well-being are always the top priorities.
Case Examples/Scenarios: Illustrating Surgical Approaches
To provide a clearer picture of how different mastopexy techniques are applied, let’s consider some hypothetical, generalized patient scenarios. These examples illustrate how the degree of ptosis and the patient’s anatomy influence the surgical plan.
Scenario 1: Mild Ptosis, Peri-Areolar Lift Candidate
- Patient Profile: A 35-year-old woman who has had one pregnancy and breastfeeding experience. She notices a slight drooping of her breasts, and her nipples point slightly downwards, but they remain above the inframammary fold. Her areolas are slightly stretched. Her skin has good elasticity. She is primarily bothered by the loss of upper pole fullness and the downward pointing nipples. She desires the least visible scarring.
- Surgical Assessment: Grade I or pseudoptosis. Good skin elasticity. Minimal excess skin.
- Recommended Technique: Peri-areolar mastopexy.
- Rationale: The limited degree of ptosis and good skin elasticity make this technique sufficient to achieve a modest lift and areola reduction. The scar is confined to the areola, meeting her preference for minimal scarring.
- Expected Outcome: A modest lift of the nipple, reduction in areola size, and some improvement in upper pole fullness. The change in shape will be subtle compared to techniques used for more severe ptosis.
Scenario 2: Moderate Ptosis, Vertical Lift Candidate
- Patient Profile: A 45-year-old woman who has gone through menopause and has experienced the effects of aging and gravity. Her nipples are at the level of the inframammary fold, and a significant portion of her breast tissue is below the fold. Her areolas are moderately stretched. Her skin elasticity is fair. She desires a noticeable lift and improvement in breast shape. She is willing to accept a vertical scar.
- Surgical Assessment: Grade II ptosis. Moderate excess skin and tissue descent. Fair skin elasticity.
- Recommended Technique: Vertical mastopexy.
- Rationale: The vertical technique allows for sufficient skin removal and reshaping to address the moderate ptosis and significantly lift the nipple above the IMF. The vertical scar allows for good control over the shape of the lower breast pole and improves projection.
- Expected Outcome: A significant lift of the breasts and nipples, improved breast shape and projection, and reduction in areola size. A vertical scar will be present from the areola to the IMF.
Scenario 3: Severe Ptosis, Inverted T Lift Candidate
- Patient Profile: A 55-year-old woman who has experienced multiple pregnancies, significant weight loss, and the effects of gravity over many years. Her nipples are significantly below the inframammary fold and are the lowest point of her breast. Her breasts are elongated and pendulous. Her skin is lax with poor elasticity. She desires a dramatic lift and a significant improvement in breast shape and firmness. She understands that this will involve more extensive scarring.
- Surgical Assessment: Grade III ptosis. Significant excess skin in all dimensions. Poor skin elasticity.
- Recommended Technique: Inverted T mastopexy.
- Rationale: The severe ptosis and excess skin in all directions necessitate the inverted T technique to achieve adequate lift, skin removal, and breast reshaping. This technique provides the greatest control over breast contour and projection for significant sagging.
- Expected Outcome: A dramatic lift of the breasts and nipples to a youthful position, significant improvement in breast shape and firmness. Scars will be present around the areola, vertically to the IMF, and horizontally along the IMF.
Scenario 4: Ptosis with Volume Loss, Mastopexy with Augmentation Candidate
- Patient Profile: A 40-year-old woman who has lost a significant amount of weight. She has moderate ptosis (nipples at the level of the IMF) and a noticeable loss of breast volume, making her breasts appear deflated. She desires a lift as well as a restoration of fullness, particularly in the upper pole.
- Surgical Assessment: Grade II ptosis with significant volume deficit.
- Recommended Technique: Vertical mastopexy with breast augmentation (implant placement).
- Rationale: The mastopexy addresses the sagging and reshapes the breast, while the implant restores the lost volume, creating a fuller and more projected appearance, especially in the upper pole. The vertical technique is often suitable for the mastopexy component in these cases.
- Expected Outcome: A lifted and reshaped breast with increased volume and fullness. Scars from the vertical mastopexy will be present, plus potential additional scarring depending on the implant insertion site (often through the IMF incision in this combined procedure).
These scenarios are simplified but illustrate how the surgeon’s assessment of the degree of ptosis and other anatomical factors directly leads to the selection of the appropriate surgical technique to best address the patient’s concerns and achieve the desired outcome.
The Role of Technology
Technology plays an increasingly important role in modern plastic surgery, including breast lift procedures. While the fundamental surgical techniques rely on anatomical understanding and manual skill, technology enhances planning, execution, and patient communication.
3D Imaging in Consultation
Advanced 3D imaging systems are becoming more common in plastic surgery consultations. These systems can:
- Create a 3D simulation of the patient’s breasts.
- Allow the surgeon to demonstrate potential outcomes with different surgical techniques and implant sizes (if augmentation is considered).
- Facilitate communication between the surgeon and patient regarding desired shape, size, and position.
- Help manage patient expectations by providing a visual representation of potential results.
While 3D imaging is a helpful tool, it is important to remember that the simulations are not a guarantee of the exact surgical outcome, as individual healing varies. However, they can significantly improve the consultation experience and aid in collaborative decision-making.
Anesthesia Monitoring Technology
Modern anesthesia involves sophisticated monitoring equipment that continuously tracks the patient’s vital signs (heart rate, blood pressure, oxygen saturation, end-tidal CO2, etc.) during the procedure. This technology allows the anesthesiologist to ensure the patient’s safety and make immediate adjustments to the anesthesia as needed.
Surgical Instruments and Techniques
Advances in surgical instrumentation have also contributed to improved safety and precision in mastopexy. These include:
- Harmonic Scalpels or Electrocautery: These tools can be used to cut tissue and simultaneously cauterize (seal) blood vessels, reducing bleeding and improving visibility during the procedure.
- Specialized Retractors: Instruments designed to hold tissues open and provide clear visualization of the surgical field.
- Advanced Suturing Materials: Improved suture materials that are strong, biocompatible, and designed to minimize tissue reaction and promote optimal healing.
While technology enhances the process, the surgeon’s skill and judgment remain the most critical factors in a successful breast lift surgery.
Antalya Specifics Expanded: Delving Deeper into the Destination
For those considering breast lift surgery in Antalya, a more detailed understanding of the local medical landscape and practicalities is beneficial.
Accreditation Bodies for Hospitals/Clinics in Turkey
When researching facilities in Antalya, look for accreditations that indicate adherence to quality and safety standards. Beyond Turkish national standards, some facilities may hold international accreditations:
- Joint Commission International (JCI): This is a globally recognized accreditation that signifies a commitment to high standards of patient care and safety. Many leading hospitals in Turkey, including some in Antalya, are JCI accredited.
- ISO Certification: While not specific to healthcare quality like JCI, ISO certifications (e.g., ISO 9001) indicate that a facility has implemented a quality management system.
Checking for these accreditations can provide an extra layer of confidence in the facility’s standards.
Experience Levels of Plastic Surgeons in Turkey/Antalya
Turkey has a strong reputation for plastic and reconstructive surgery, with many surgeons receiving extensive training both domestically and internationally. The field is popular and competitive, leading to a high level of expertise among many practitioners. When researching surgeons in Antalya, look for:
- Membership in Turkish Society of Plastic, Reconstructive and Aesthetic Surgeons (TSPRAS): This is the main professional body for plastic surgeons in Turkey.
- Membership in International Societies: Membership in organizations like the European Association of Plastic Surgeons (EURAPS) or the American Society of Plastic Surgeons (ASPS) (though this requires US-based practice, many Turkish surgeons have trained or observed in the US) indicates engagement with international standards and ongoing education.
- Publications and Presentations: A surgeon who publishes research or presents at conferences demonstrates a commitment to advancing the field and staying current with best practices.
Don’t hesitate to ask about the surgeon’s training, experience, and specialization during the consultation.
Post-Operative Care Packages and Facilities Available in Antalya
Many clinics and medical tourism facilitators in Antalya offer comprehensive packages that go beyond the surgery itself. These can include:
- Accommodation: Stays in comfortable hotels, sometimes with specialized post-operative care services available.
- Airport Transfers: Transportation to and from the airport.
- Patient Coordinators: Staff who assist international patients with logistics, scheduling, and communication.
- Nursing Support: Access to nursing care at your accommodation during the initial recovery phase.
- Transportation to Appointments: Arranging transport for follow-up visits.
These packages can significantly simplify the logistics of undergoing surgery abroad and provide a supportive environment for recovery. However, carefully review what is included in the package and ensure it meets your needs.
Combining Surgery with a Recovery Vacation: Pros and Cons
Antalya’s appeal often includes the opportunity to combine surgery with a holiday. While the idea of recovering in a beautiful location is attractive, it’s important to be realistic about the recovery process.
- Pros: A relaxing environment can reduce stress and contribute to a more positive recovery experience. Having a dedicated period away from daily life allows you to focus solely on healing.
- Cons: Recovery from breast lift surgery involves discomfort, swelling, and limited mobility. You will not be able to engage in typical tourist activities (swimming, sightseeing, strenuous excursions) during the initial recovery period. It’s crucial to prioritize rest and healing over vacation activities. Ensure your accommodation is suitable for recovery and that you have access to any necessary support.
If you plan to combine surgery with a vacation, schedule the more active vacation portion after you have received full clearance from your surgeon to resume all activities, which is typically several weeks to months post-surgery. The initial period in Antalya should be focused purely on rest and recovery.
Long-Term Follow-Up
My commitment to my patients extends beyond the operating room and the immediate post-operative period. Long-term follow-up is an essential part of ensuring the ongoing health and aesthetic outcome of your breast lift surgery.
Importance of Scheduled Follow-Up Visits
While initial follow-up appointments are focused on wound healing and early recovery, subsequent visits allow me to monitor the long-term results.
- Assessing Scar Maturation: I evaluate how your scars are healing and maturing over time and can provide further recommendations for scar management if needed.
- Monitoring for Late Complications: While rare, some complications can manifest weeks or months after surgery. Follow-up visits allow for early detection and management of issues like seroma formation, fat necrosis, or significant asymmetry that develops over time.
- Evaluating Long-Term Aesthetic Outcome: I assess the long-term shape, position, and symmetry of your breasts to ensure the results are stable and satisfactory.
- Addressing Concerns: Follow-up appointments provide an opportunity for you to discuss any lingering questions or concerns you may have about your breasts or the surgical outcome.
Even if you are feeling well, attending scheduled follow-up appointments is important for ensuring the best possible long-term results and addressing any potential issues proactively.
Addressing Concerns Over Time
Changes in your breasts can occur over time due to natural aging, weight fluctuations, or other factors. If you notice any significant changes in the shape, size, or feel of your breasts, or if you have any concerns about your scars or sensation, it is important to contact my office. While some changes are normal, others may warrant evaluation to rule out complications or address aesthetic concerns.
Maintaining open communication with your surgeon throughout the years following your mastopexy is beneficial for your long-term satisfaction and breast health.
Comparing Techniques: Pros and Cons
Choosing the right mastopexy technique is a balance between the desired amount of lift and reshaping and the associated scar burden. Here’s a comparison of the main techniques from a practical perspective:
| Feature | Peri-Areolar (Donut) Mastopexy | Vertical (Lollipop) Mastopexy | Inverted T (Anchor) Mastopexy |
| Degree of Ptosis | Minimal (Grade I or Pseudoptosis) | Mild to Moderate (Grade I and II) | Moderate to Severe (Grade II and III) |
| Amount of Lift | Modest | Moderate to Significant | Significant to Dramatic |
| Reshaping Capability | Limited | Good control over lower pole and projection | Excellent control over entire breast mound and projection |
| Scarring | Confined to the areola (least visible) | Around the areola plus a vertical scar to the IMF | Around the areola, vertical scar, and horizontal scar in the IMF (most visible) |
| Ideal for | Patients with minimal sagging, good skin elasticity, and a strong desire for minimal scarring. | Patients with mild to moderate sagging and who are willing to accept a vertical scar for a better lift and shape. | Patients with moderate to severe sagging requiring significant skin removal and reshaping, where the benefits of the lift outweigh the more extensive scarring. |
| Potential Issues | Limited lift, potential for areola widening, slight flattening. | Vertical scar healing, potential for some residual fullness below the IMF in larger breasts. | Most extensive scarring, potential for healing issues at the junction of the scars (triple junction), longer scar maturation time. |
This comparison highlights that the “best” technique is subjective and depends entirely on the individual patient’s anatomy, the severity of their ptosis, and their priorities regarding scarring versus the degree of lift and reshaping. During the consultation, I discuss these trade-offs with the patient, explaining why a particular technique is recommended for their specific case.
The Future of Mastopexy
The field of plastic surgery is constantly evolving, with ongoing research and development aiming to improve techniques, minimize scarring, and enhance outcomes. While traditional mastopexy techniques remain the gold standard for most cases of significant ptosis, future advancements may include:
Advances in Techniques
Refinements in existing surgical techniques, such as improved methods for glandular plication or more precise approaches to NAC pedicle design, continue to evolve based on surgeon experience and outcomes research.
Minimally Invasive Approaches
While challenging for significant ptosis, there is ongoing exploration into less invasive methods for breast lifting. These might involve:
- Thread Lifts: Using specialized sutures or threads inserted under the skin to provide a modest lift. Currently, thread lifts offer a much less significant and less durable lift than traditional mastopexy and are generally only suitable for very minimal sagging.
- Radiofrequency or Ultrasound Devices: Technologies that use energy to heat and tighten skin tissue. These can provide some skin tightening but are not a substitute for surgical skin removal and reshaping in cases of moderate to severe ptosis.
These minimally invasive approaches are currently limited in their effectiveness for significant ptosis but may offer options for very mild cases or as adjuncts to surgery in the future.
Tissue Engineering
In the more distant future, advancements in tissue engineering could potentially offer new ways to regenerate or reinforce breast tissue and ligaments, potentially providing alternative or supplementary approaches to surgical lifting. However, this is still largely in the realm of research.
While the core principles of mastopexy have been established for many years, the pursuit of safer, more effective, and less scarring techniques continues to drive innovation in the field.
Conclusion: Achieving Perkier Breasts in Antalya
In conclusion, breast lift surgery (mastopexy) is a transformative procedure that can effectively address breast ptosis, restoring a more youthful, elevated, and aesthetically pleasing breast contour. As a plastic and reconstructive surgeon, I have witnessed firsthand the positive impact this surgery can have on a woman’s self-confidence and quality of life.
The decision to undergo a breast lift is a personal one, requiring careful consideration and realistic expectations. A thorough consultation with an experienced and qualified plastic surgeon is the essential first step. During this consultation, your anatomy will be assessed, your goals will be discussed, and a personalized surgical plan will be developed, taking into account the degree of ptosis and your desired outcome versus the associated scarring.
Understanding the various surgical techniques – from the peri-areolar for minimal lifts to the inverted T for significant reshaping – allows you to appreciate the rationale behind the recommended approach for your specific needs. Furthermore, being informed about the potential risks and the recovery process is crucial for a smooth and successful journey.
For those considering breast lift surgery in Antalya, Turkey offers a compelling combination of factors: access to experienced and highly qualified surgeons, modern and accredited medical facilities, and competitive costs, all within a favorable environment for recovery. However, diligent research in selecting your surgeon and clinic, coupled with meticulous planning for your medical trip, is paramount to ensuring a safe and positive experience.
Achieving perkier breasts through mastopexy can significantly enhance your appearance and boost your self-esteem. By choosing a skilled surgeon, undergoing a comprehensive evaluation, and having realistic expectations, you can embark on this journey with confidence, knowing that you are taking a significant step towards feeling more comfortable and positive about your body. Whether you choose to have your procedure locally or in a medical tourism destination like Antalya, prioritizing your safety, informed consent, and selecting an experienced surgeon dedicated to achieving natural-looking, harmonious results are the cornerstones of a successful breast lift.
Transform Your Confidence with Surgyteam!
Join the thousands of satisfied patients who have experienced the exceptional care and expertise of Surgyteam’s renowned plastic surgeons. Whether you’re seeking aesthetic enhancements or reconstructive surgery, our dedicated team in Antalya is here to provide you with the highest quality treatment and personalized care.


